Top 22 Healthcare Revenue Cycle Management Solutions To Reduce Denials in 2026
Explore our top picks for 22 top revenue cycle management solutions to help healthcare RCM teams reduce denials and get more cash flow.
January 7, 2026


If there’s one quote that applies to healthcare revenue cycle teams today more than almost any other group, it’s “Work smarter, not harder!” Coding backlogs, prior auth delays, payer rules that never stop changing—RCM work has a way of consuming entire days.
Amid all the chaos RCM teams deal with, the right revenue cycle management solutions can feel like a lifeline.
Thanks to AI and automation booming at a mile a minute, today’s RCM solutions automate the slow parts, simplify the confusing parts, and clean up the messy parts. Some handle eligibility in seconds, others flag documentation gaps before they cause trouble, and a few can even pick up the phone and call payers so your team doesn’t have to.
To make it easier for you to find the RCM solutions for your organization, here’s a breakdown of 22 high-impact healthcare revenue cycle solutions—organized across front-end, mid-end, and back-end RCM.
Front-End RCM
Front-end RCM covers every administrative and financial activity that happens before a patient receives care. These early steps set the foundation for clean claims, accurate billing, and smooth downstream workflows.

This stage is all about capturing the right information upfront, and aligning payer requirements early, long before it ever reaches billing.
Here are the key components of front-end RCM:
- Patient scheduling: Managing appointment workflows efficiently so providers, staff, and patients are aligned before the visit.
- Patient registration and pre-registration: Collecting accurate demographic, insurance, and clinical intake information ahead of time to minimize errors later.
- Insurance eligibility and benefits verification: Confirming coverage, benefits, deductibles, and plan rules to prevent eligibility-related denials.
- Prior authorization management: Payer's pre-approval for specific medical services, treatments, or procedures.
- Patient responsibility estimation: Helping patients understand expected out-of-pocket costs, available payment options, and financial obligations before care is delivered.
Let’s look at our top picks for front-end RCM solutions:
1. PracticeSuite: For Effortless Patient Scheduling
PracticeSuite is a fully integrated practice management platform that streamlines front-end RCM tasks like scheduling, patient registration, and insurance verification. It mainly caters to small-to mid-sized independent practices.
A standout benefit PracticeSuite offers is its modular pricing structure (pay only for what you need), which helps smaller practices avoid high upfront costs.
The system’s scheduling module is designed to support high-volume practices with features like:
- Drag-and-drop calendars
- Automated reminders
- Waitlists
- Recurring appointments
- Multi-location scheduling
- Built-in eligibility checks
2. DIVA 360°: Dezy It’s Voice & Conversational AI Platform
DIVA 360° is Dezy It’s enterprise-grade Voice and Conversational AI platform built specifically for multi-location aesthetic clinics and wellness chains.
DIVA captures inbound patient demand and actively follows up on outbound leads from ads, social media, website chat, and phone calls. Using natural, conversational interactions, without relying on rigid forms, DIVA qualifies intent, answers questions, and books appointments inline while syncing data directly into CRMs and EHRs.
Core capabilities include:
- Inbound Voice AI that answers calls, qualifies patients, and books appointments 24/7
- Outbound Voice AI that follows up with leads across all acquisition channels, converting
them seamlessly - Conversational web chat that enables inline booking
- Capture clean, structured patient data instantly with real-time EHR and CRM integration
By unifying voice, chat, and follow-up into a single system, DIVA 360° helps aesthetic clinics convert more leads without increasing operational complexity.
3. NextGen: All-in-one patient engagement hub
NextGen’s Patient Portal markets its platform to ambulatory and specialty practices as well as larger provider organizations that need a specialty-aware EHR + patient experience suite. The platform connects patients and practices via:
- Secure messaging
- Access to results and records
- Online appointment scheduling
- Prescription renewals
- Integrated payments
4. CombineHealth’s Mark AI for Eligibility Verification
Mark is CombineHealth’s autonomous medical billing and eligibility agent, designed to remove the manual burden of payer portal work. The AI agent navigates 50+ payer portals and aggregators to perform real-time eligibility checks to:
- See if the patient has active insurance coverage
- Verify benefits information, including copayments, deductibles, co-insurance percentages, and specific coverage limitations
- Retrieve secondary insurance information (if applicable)
Case Study: How CombineHealth helped reduce the eligibility verification time by 80% for an anesthesia group
5. CohereHealth for Clinical-Intelligence Prior Authorization
CohereHealth offers a clinical-grade AI solution that automates and simplifies prior authorization for providers and utilization management for payers. It’s basically a platform that providers use when the payer has bought and implemented it. Here’s how the platform works for providers:
- Providers submit prior auth requests digitally to a specific health plan
- The platform uses AI + clinical guidelines to auto-approve a large share of requests and route the rest to human reviewers
- It also integrates with EHRs, Epic Payer Platform, and CMS-0057-F APIs, so providers can get requirements, send requests, and see decisions more smoothly
Its key offerings include its digital-first intake (web intake, EHR submission, phone/fax fallback), clinical-data extraction, and intelligent pre-population to reduce manual burden.
6. CombineHealth’s Stephanie AI: An AI Prior Authorization Agent
Stephanie is CombineHealth’s upcoming AI prior authorization specialist, built specifically for providers and billing teams. Here’s how the AI agent works:
- Detects when an authorization is needed by checking payer rules, benefits, diagnosis, and procedure codes
- Pre-populates forms with all required demographics and clinical details
- Submits requests across 70+ payer portals
- Monitor each case around the clock and escalate stalled requests
- Places phone calls to payer representatives when necessary
While CohereHealth’s core strength is AI decisioning that matches requests to payer policies, Stephanie’s forte lies in the automated execution of PA workflows.
7. PMMC: Financial Counselling & Patient Responsibility Estimation
PMMC’s Patient Estimates software helps healthcare providers provide patients with accurate out-of-pocket cost estimates based on their insurance coverage and the specific services to be rendered.
The platform is web-based, integrates with providers’ contract management platforms and is maintained by PMMC.
The company mainly caters to hospitals and health systems, particularly oncology centers like Moffitt Cancer Center, but is applicable across various provider types to help with price transparency regulations, such as the No Surprises Act.
Some of its standout features include:
- Accurate cost estimation based on actual payer contract data
- Compliance with federal price transparency mandates
Mid-End RCM
Mid-end RCM is where clinical activity is translated into billable, compliant claims. This stage focuses on accuracy, documentation integrity, and ensuring every service delivered is correctly captured and justified.
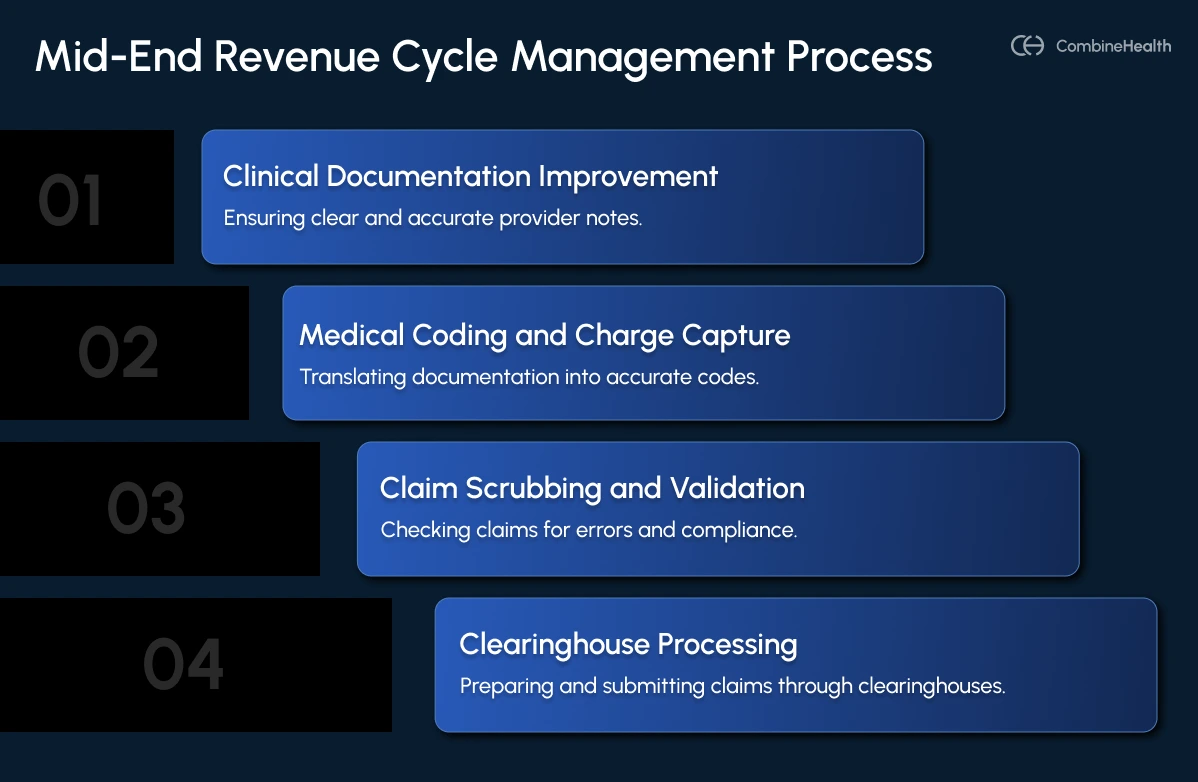
Here are the key components of mid-end RCM:
- Clinical documentation improvement: Ensuring provider notes clearly reflect diagnoses, procedures, medical necessity, and the full complexity of care so claims can be coded correctly.
- Medical coding and charge capture: Translating clinical documentation into accurate ICD-10, CPT, HCPCS, and E/M codes while capturing all billable services, procedures, and supplies.
- Claim scrubbing and validation: Running claims through edits and payer rules to catch errors, validate compliance, correct missing data, and prepare clean claims for submission through clearinghouses.
- Clearinghouse processing: Ensuring claims are formatted, validated, and routed correctly to each payer for successful electronic submission.
8. CombineHealth’s Amy AI for Clinical Documentation Improvement
CombineHealth’s Amy AI is designed as a CDI-first AI medical coding agent that analyzes every encounter note the moment it lands in the EMR.
Here’s what makes Amy AI a perfect CDI solution:
- Holistic CDI + coding + claims auditing solution
- Identifies missing specifics, unclear diagnoses, and documentation elements that could cause denials later
- Autonomously assigns correct ICD-10, CPT, and E/M levels, adjusting to payer-specific rules and guidelines
- Delivers a line-by-line rationale for every code so coders, auditors, and providers understand why it was selected
- Highlights complex or ambiguous cases to coders, maintaining coding accuracy
.webp)
9. Solventum’s Clinical Documentation Integrity System
Solventum 360 Encompass CAC automates coding workflows using computer-assisted coding that automatically suggests medical codes based on patient documentation. It uses natural language processing (NLP) and artificial intelligence (AI) to analyze clinical records deeply and identify documentation deficiencies that matter most for compliance and reimbursement.
Some of its standout features include:
- AI-driven prioritization of cases to identify documentation deficiencies that matter most for compliance and reimbursement
- Facilitates query management, allowing teams to track, record, and respond to documentation queries efficiently
- Supports expanding CDI programs across multiple care settings while maintaining core responsibilities
- Integrates with Solventum’s coding and auditing systems
10. 3M 360 Encompass Computer-Assisted Coding Solution
3M’s CAC solution is designed to free coders from manual data organization by analyzing clinical documentation to auto-suggest accurate diagnosis/procedure codes (ICD-10, CPT) with evidence-based rationale. It particularly caters to large hospitals and health systems with high-volume inpatient/outpatient coding needs.
Some of its best offerings include:
- Integration with 3M CRS, CDI, auditing, and cloud/on-premises deployment via AWS
- Advanced code sequencing, concurrent coding, and single-path outpatient workflows
11. Find-A-Code: A Code Search Platform
Find-A-Code is an intuitive code search platform that helps medical coders to quickly locate, validate, and crosswalk medical codes across major systems, including ICD-10-CM/PCS, CPT, and HCPCS. Every search query offers details like code descriptions, guidelines, modifiers, Medicare fee schedules, and validation to ensure compliance and billing accuracy.
It’s a handy tool for medical coders, billers, auditors, and healthcare providers (e.g., physicians, clinics) needing quick code lookup and validation.
12. CombineHealth’s Amy AI: Autonomous Coding With Human-in-the-Loop Approach
Amy is CombineHealth’s CDI-aware, AI-powered medical coding agent designed to autonomously generate medical codes, with supervised autonomy built into her design. Here’s how she works:
- Reads full encounter data directly from the EHR, including notes, vitals, labs, operative reports, consults, and discharge summaries
- Uses NLP and transformer-based models to understand clinical context
- Assigns highly accurate codes across all major code sets
- Explains every coding decision she makes
- Only routes complex or low-confidence charts to human coders
Amy is built with the realities of modern coding teams in mind. She’s designed to help hospitals and health centers, and multi-specialty and speciality groups needing high-volume, high-accuracy autonomous coding plus CDI support.
.webp)
13. CombineHealth’s Mark AI: Medical Billing & Claim Scrubbing
Mark is CombineHealth’s always-on AI medical billing agent that automates end-to-end billing workflows—from claims generation and submission to ERA/EOB reading, payment posting, and reconciliation. Here’s how Mark operates:
- Automatically fills out CMS-1500 and UB-04 claim forms
- Performs real-time eligibility verification and benefits checks
- Submits claims with built-in error checks across 50+ payer portals
Additionally, Mark learns from prior denial patterns and integrates directly with billing software to eliminate manual data entry errors.
14. Office Ally Clearinghouse
OfficeAlly offers a comprehensive clearinghouse solution, helping hospitals, health plans, and high-volume submitters streamline claims processing. It offers electronic claims submission and payment processing services with real-time insurance eligibility verification.
Some of its standout features are:
- Real-time status alerts and email notifications for claims and payments
- Toolset to minimize rejections through payer verification and clean claim submission
15. Stedi: API-First Clearinghouse
Stedi is an API-first, programmable clearinghouse built for modern RCM to scale automation for eligibility checks, claims submission, and ERAs. This allows health tech companies to build superior products without legacy EDI compromises.
Here’s what the platform offers:
- Handles all major healthcare transactions: batch/real-time eligibility, claims submission with automated edits, and ERAs with streamlined enrollment
- Provides developer-friendly APIs for programmatic integration, real-time tracking, error detection, and transaction management
- Automates EDI processes end-to-end, with customizable dashboards for monitoring claims status and resolving issues
Back-End RCM
Back-end RCM is where submitted claims turn into actual revenue. Once a claim leaves the clearinghouse, the back-end team ensures payments are posted correctly, denials are analyzed and overturned, and outstanding balances are collected.
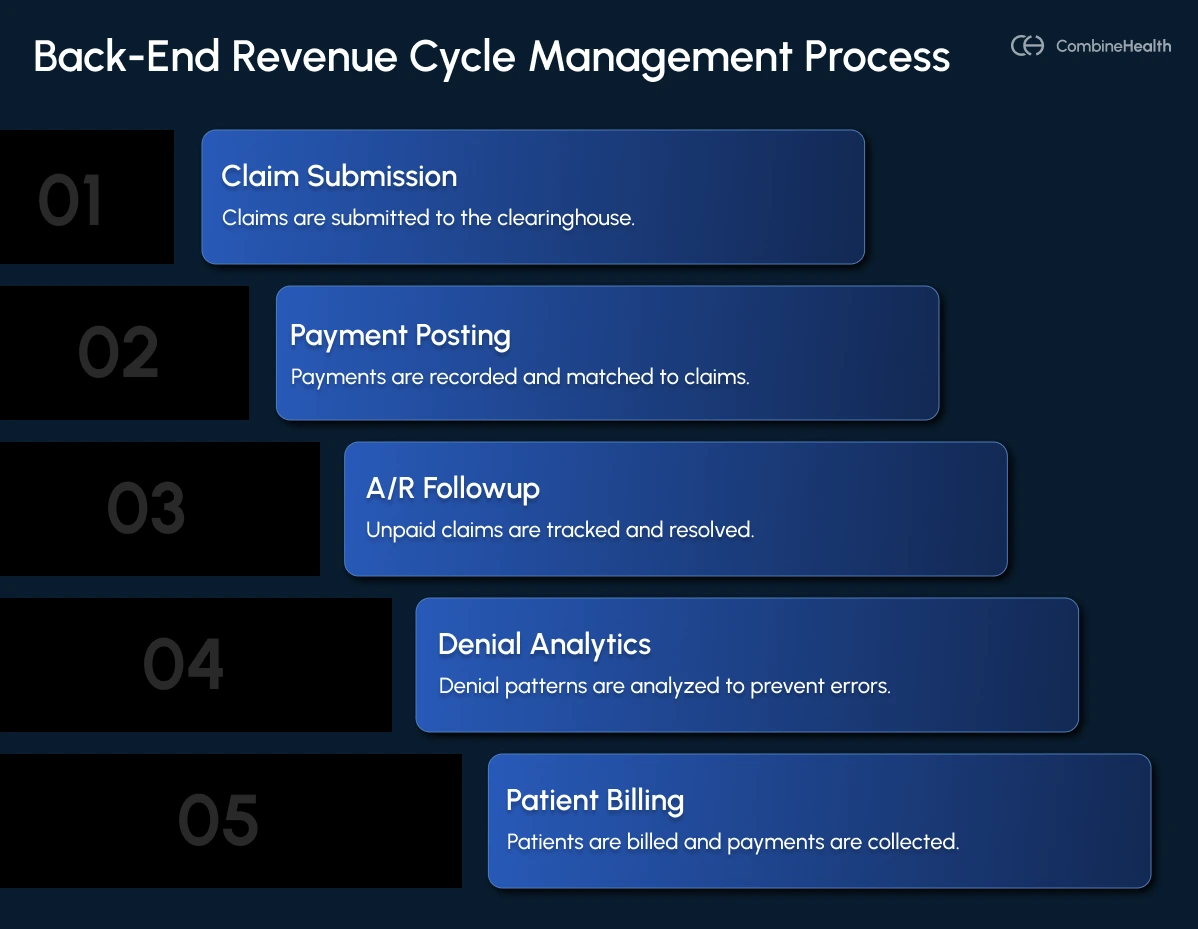
Here are the core components of back-end RCM:
- Payment posting and ERA processing: Recording payer remittances accurately, matching payments to claims, and identifying underpayments or discrepancies.
- A/R followup: Tracking unpaid claims, contacting payers, resolving delays, and ensuring every claim is actively worked until payment is received.
- Denial analytics: Identifying patterns behind denials, pinpointing root causes, and informing upstream process improvements to prevent repeat errors.
- Patient billing and self‑pay collections: Sending accurate patient statements, offering payment options, and collecting outstanding balances while maintaining a positive patient experience.
16. eClinicalworks: Payment Posting & Electronic Remittance Advice (ERA) Processing
eClinicalWorks RCM delivers comprehensive back-end billing, including claims scrubbing/submission, ERA posting, denials/appeals management, patient eligibility checks, and AR aging prioritization. Its key features include:
- Dynamic dashboards
- Work queues
- Provider analytics
- Self-service practice management
- Performance KPIs to track claims status, timely filing risks, and financial health
17. CombineHealth’s Mark AI: Payment Posting and Reconciliation
CombineHealth’s Mark automates payment posting and reconciliation at scale, which involves:
- Reading ERAs/EOBs in real time
- Matching payments to claims with 99%+ accuracy
- Reconciling totals automatically
- Flagging discrepancies
The AI agent posts payments directly to patient accounts and insurance adjustments in billing software, eliminating manual data entry and reconciliation delays. Plus, you get real-time visibility into payment status, A/R aging, and collection rates by payer and procedure to prevent payment leakage.
Recommended Reading: How Mark AI generates 150+ claims in minutes for an anaesthesia group
18. CombineHealth’s Adam AI for A/R Follow
Adam is CombineHealth’s advanced AI denial management solution that automates denial detection, root cause analysis, and resolution workflows. Here’s how Adam operates a denial management workflow:
- Continuously monitors claim statuses across payer portals to instantly identify denial patterns and root causes
- Automates A/R follow-ups, including AI-driven phone calls navigating IVRs and live agents, recording call summaries, and recommending next steps to resolve denials
- Prioritizes denials based on age, dollar value, payer, and likelihood of recovery, using customizable workflows and payer scorecards
- Tracks appeal deadlines, manages submissions, and pressures payers with automated, smart appeal letter drafting
- Provides real-time dashboards with denial trends, case statuses, and predictive analytics
19. CombineHealth’s Rachel AI: Appeals Management
CombineHealth’s Rachel automates and accelerates medical appeals by drafting clear, payer-specific appeal letters using clinical documentation and payer rules. Here’s how she operates:
- Generates evidence-based appeals for medical necessity, coding, and coverage denial reasons
- Uses machine learning to predict the most effective appeal strategies and manages deadlines and escalation workflows
- Extracts subtle clinical documentation references to strengthen appeal arguments
- Integrates with EHR, practice management, and billing systems for smooth workflow integration
20. CombineHealth’s Penny AI: Policy Review
CombineHealth’s Penny ensures claims are compliant with up-to-date payer policy by continuously monitoring thousands of payer rules, reducing denials by predicting non-compliant claims before submission. Here’s how:
- Reviews claims for alignment with Medicare, Medicaid, and commercial payer policies
- Predicts denial risks from policy mismatches and alerts teams pre-submission
- Automates policy monitoring with real-time updates and customizable dashboards
21. CombineHealth’s Taylor: Denial Dashboard
CombineHealth’s Taylor Denial analytics delivers real-time, AI-powered insights and analytics across the entire RCM process, showing the overall health of an organization’s RCM. Here’s how it works:
- Continuously analyzes charge capture, claims submission, first-pass acceptance, A/R aging, and collections performance
- Provides KPI dashboards, payer scorecards, contract monitoring, and staff productivity analytics for providers and teams
- Uses machine learning to forecast cash flow and highlight revenue leakage before it occurs
- Enables natural language querying of RCM data for tailored reports and insights
22. Billie by Collectly: Patient Billing & Self‑Pay Collections
Collectly’s Billie is a 24/7 AI agent that instantly resolves patient billing questions, disputes, and payments across voice, chat, text, email, and web. Here’s what it does:
- Pulls real-time data from EHR/PM systems to answer patient queries with context-aware responses in multiple languages
- Clarifies bills, sets up self-serve payment plans/options, updates insurance/contact details via secure API, and verifies eligibility/benefits
- Escalates complex issues to staff
- Handles omnichannel patient engagement (voice calls navigating scenarios, chat/text/email)
CombineHealth’s AI Agents: The Best End-to-End Customizable RCM Solution for Reducing Denials
CombineHealth’s specialized AI workforce automates the entire revenue cycle through interconnected agents working sequentially across front-end, mid-end, and back-end RCM. Each agent handles specific tasks with explainable decisions, human-in-the-loop escalation, and seamless EHR/PM integration.
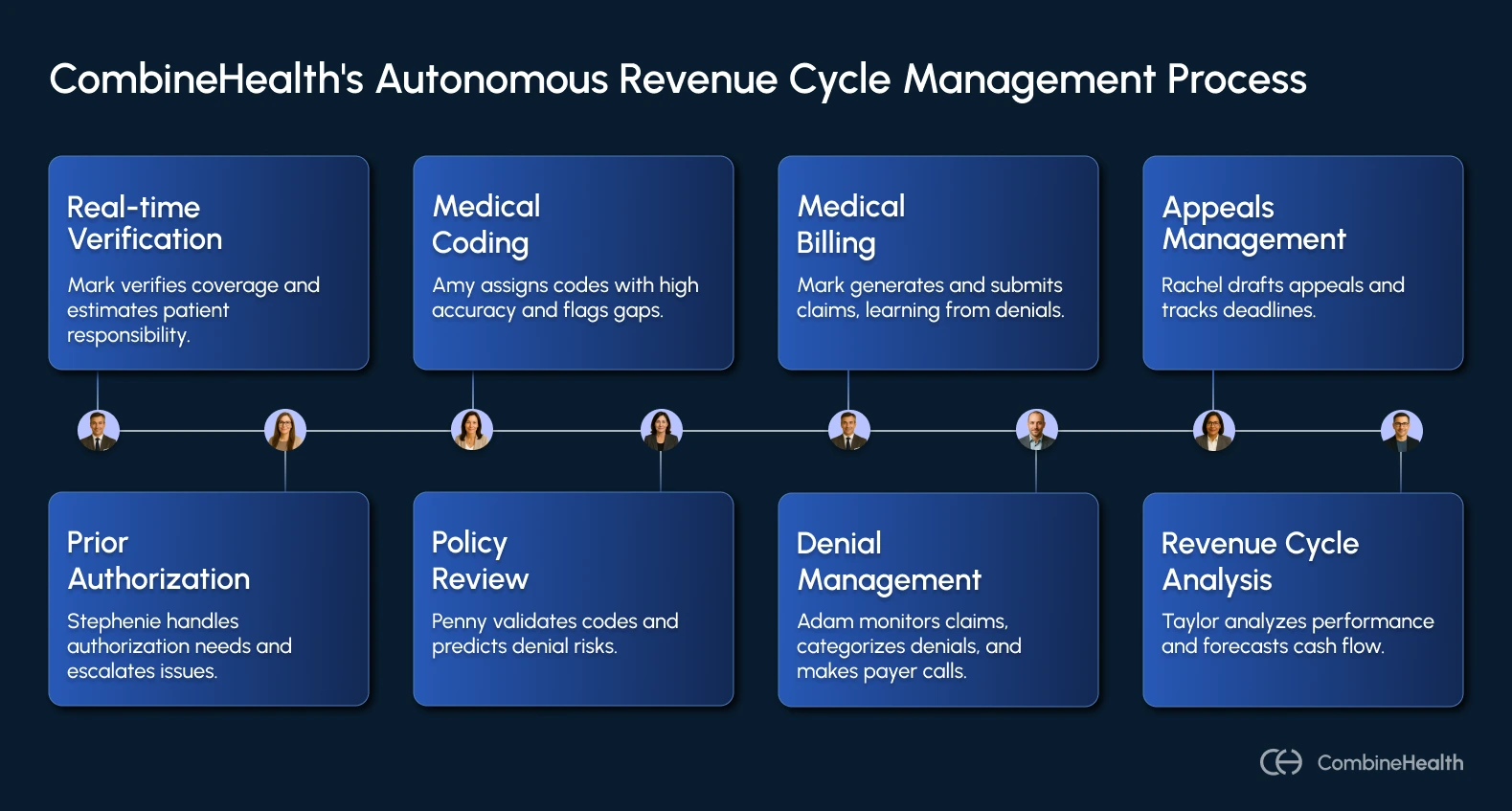
Here’s how they work autonomously together:
- Mark (AI Billing Agent) performs real-time verification across 50+ payer portals, confirming coverage, deductibles, copays, and secondary insurance while estimating patient responsibility.
- Stephanie (AI Prior Auth Agent) detects authorization needs from notes/codes, pre-populates forms, submits via portals/phone/fax, and monitors/escalates stalled requests.
- Amy (AI Medical Coder) ingests full EHR encounter data (notes, vitals, labs, reports), assigns ICD-10/CPT/E/M/HCPCS codes with 99%+ accuracy, provides line-by-line rationale/guideline citations, and flags CDI gaps or escalates complex cases.
- Penny (AI Policy Reviewer) validates codes against CMS manuals/payer policies (LCDs/NCDs, frequency edits), predicts denial risks with page-level citations, and alerts for pre-submission fixes.
- Mark (AI Medical Biller) generates CMS-1500/UB-04 forms, scrubs claims with payer-specific edits, submits via clearinghouses/portals, and learns from prior denials.
- Adam (AI Denial Manager) monitors claim status across portals, categorizes denials (clinical/coding/eligibility), prioritizes by value/age, makes AI-driven payer calls (IVR/live agents), records summaries, and recommends next steps.
- Rachel (AI Appeals Manager) drafts payer-specific appeal letters with evidence extraction from notes, predicts success probability, adapts to organizational style, and tracks deadlines/escalations.
- Taylor (AI Revenue Cycle Analyst) analyzes end-to-end performance (KPIs, payer scorecards, A/R aging, bottlenecks), forecasts cash flow leakage, generates custom reports, and feeds insights back to upstream agents.
Ready to Reduce Your Claim Denials?
The RCM solutions highlighted in this guide show that when technology removes the repetitive work, RCM teams get to focus on higher-impact tasks that truly move the needle. So, go on demos, assess the fit and and see which solutions genuinely support your team’s goals and challenges.
If you're ready to explore how CombineHeath’s AI Agents can streamline your entire revenue cycle, book a demo with us!
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










