What Is Medical Coding, and How AI Medical Coding Can Help Reduce Claim Denials
Understand all about medical coding, its various types, and how it works. Explore how AI medical coding can help reduce denials and increase claim reimbursements.
January 5, 2026

Key Takeaways
• Translating patient visits into accurate codes ensures clinics and billing companies get paid promptly and fairly.
• Even minor coding errors can cause claim denials, payment delays, or extra administrative work.
• The main code sets (ICD for diagnoses and CPT for procedures) act as a universal language, allowing seamless communication between clinics, hospitals, and insurers.
• AI-powered coding can drastically reduce denials, speed up payments, and boost overall collections.
• AI systems, like CombineHealth’s Amy, handle routine coding decisions, flag ambiguous cases for human review, and provide real-time error checking—all while integrating with digital workflows.
Imagine a busy clinic on Monday morning. Phones keep ringing, patients fill the waiting room, and staff scramble to keep up. After appointments, there's another mountain to climb—turning the details of every visit into the right code before submitting claims to insurance companies.
The harder problem is capturing why those codes make sense.
But medical coding is not as simple as matching diseases to numbers. Even a tiny error can lead to denials, payment delays, or requests for extra information.
In this article, we’ll break down what is medical coding, how it works, and how AI can help reduce coding-related denials and rework.
.webp)
What Is Medical Coding?
Medical coding is the process of translating details from a patient's visit into standard codes. These codes are used for insurance billing, reporting, and tracking patient outcomes over time. Each diagnosis, procedure, or service gets its own code, which allows hospitals, clinics, and insurance companies to communicate clearly.
For health centers and hospitals, accurate coding isn't just about crossing T's and dotting I's. It's about getting reimbursed fairly and on time, avoiding claim rejections, and following the rules set out by insurance programs like Medicare and Medicaid.
What Are the Different Types of Medical Coding?
Medical coding encompasses several distinct coding systems, each serving specific purposes in clinical documentation and billing.
At a high level, medical coding answers three core questions:
- What condition does the patient have?
- What services or procedures were performed?
- How complex was the medical decision-making involved?
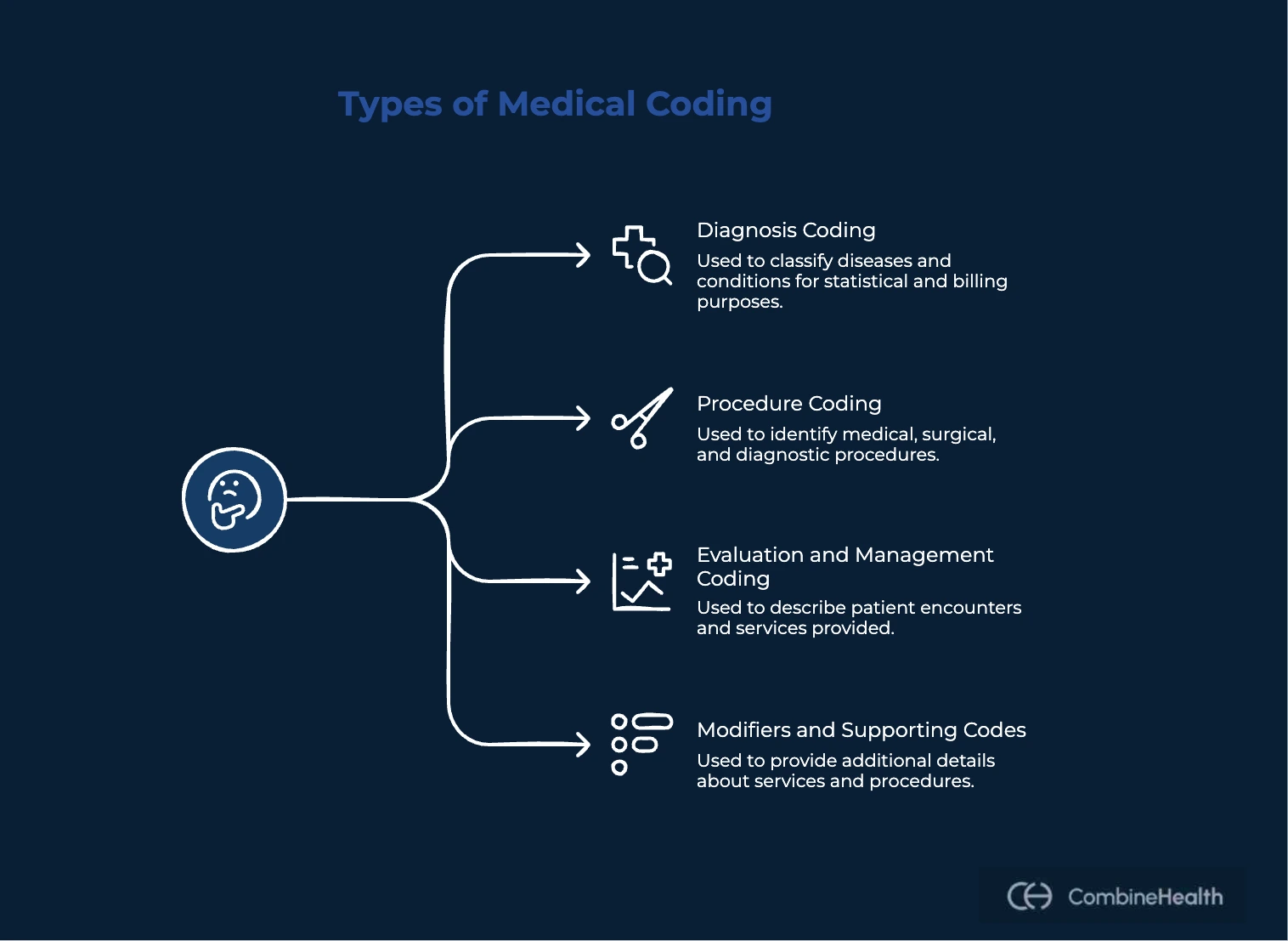
To answer these questions consistently across the healthcare system, coders rely mainly on the following standardized coding systems, each designed for a specific purpose:
Diagnosis Coding (ICD-10-CM)
Diagnosis codes describe why the patient was treated.
The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) system is used to document:
- Patient conditions and symptoms
- Acute vs. chronic illnesses
- Severity, laterality, and complications
Example:
Two patients with the same condition may require different ICD-10 codes depending on severity or associated risk factors. This makes diagnosis coding foundational not just for billing, but also for risk adjustment, quality reporting, and population health analysis.
Procedure Coding (CPT & HCPCS)
Procedure codes describe what was done during the encounter.
- CPT (Current Procedural Terminology) codes capture most physician services and procedures, such as office visits, surgeries, and diagnostic tests.
- HCPCS Level II codes are primarily used for supplies, durable medical equipment, and certain non-physician services.
Procedure coding requires careful alignment with documentation. Even when the correct service is provided, missing details—such as technique, duration, or approach—can affect whether a code is valid or reimbursable.
Evaluation and Management (E/M) Coding
E/M coding captures how complex the clinical decision-making was.
Unlike diagnosis and procedure coding, E/M coding depends heavily on clinical reasoning. It reflects:
- The number and complexity of problems addressed
- The amount and complexity of data reviewed or interpreted
- The level of risk to the patient
Two visits with similar diagnoses may result in very different E/M levels depending on the provider’s thought process, risk assessment, and data interpretation. This makes E/M coding one of the most judgment-driven and most scrutinized areas of medical coding.
Modifiers and Supporting Codes
Modifiers provide additional context about how a service was performed.
They are used to indicate:
- Distinct or separate procedures
- Professional vs. technical components
- Increased complexity or unusual circumstances
When applied correctly, modifiers ensure accurate reimbursement. When applied incorrectly or without clear justification, they are a common source of denials and audits.
Additional coding systems include DRG codes for inpatient reimbursement, NDC codes for pharmaceuticals, and specialty-specific codes like dental (CDT) or mental health coding systems. Each type serves a unique function in the healthcare revenue cycle, ensuring comprehensive documentation and appropriate reimbursement for all services provided.
How Is Computer-Assisted Coding Different from Autonomous Coding and Which Is Better?
Many healthcare organizations lump all “AI coding tools” into one category. In reality, there’s a meaningful difference between computer-assisted coding (CAC) and autonomous coding, and that difference directly affects accuracy, scalability, and compliance.
Computer-assisted coding is designed to support human coders, but it doesn't reason through the encounter end to end.
In a CAC workflow:
- The system scans clinical documentation using rules and NLP
- It suggests possible ICD-10, CPT, or HCPCS codes
- A human coder reviews, edits, accepts, or rejects those suggestions
- Final responsibility always rests with the coder
Autonomous coding takes a fundamentally different approach.
Instead of suggesting codes for human selection, autonomous systems:
- Analyze the full encounter record
- Apply coding guidelines and payer rules directly
- Generate codes independently
- Provide explicit rationale and evidence for each decision
- Escalate uncertainty to human reviewers when needed
Which Is Better: CAC or Autonomous Medical Coding?
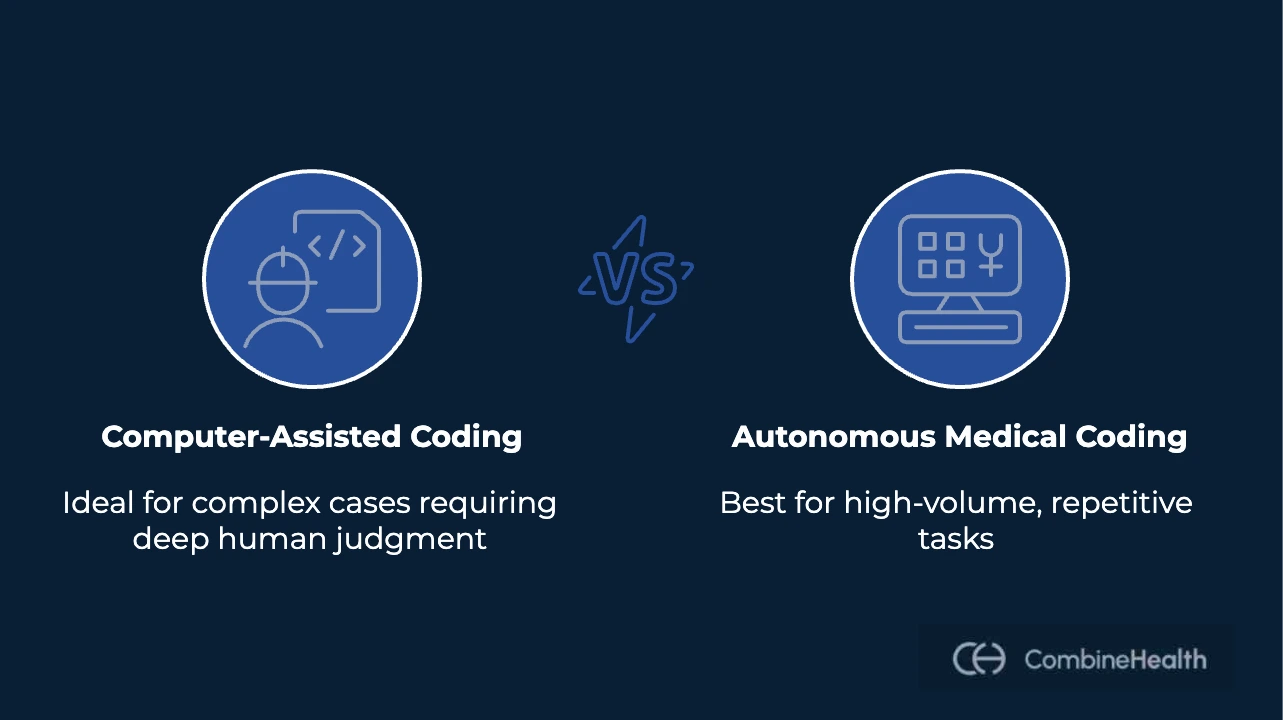
Neither approach is universally “better," but they solve different problems:
CAC is ideal to use when:
- Case volume is manageable
- Encounters are consistently complex
- Deep human judgment is required for most charts
However, autonomous medical coding is better when:
- Volume is high and repetitive
- Coding rules are well-defined
- Consistency and turnaround time matter
- Human review can be focused on exceptions
How AI Can Be Used in Medical Coding
In the past, coding relied solely on coding specialists for carefully reading notes and matching them to the right code.
Now, technology like artificial intelligence (AI) has stepped in to help. The process can be faster, more accurate, and even run 24/7. AI-powered systems analyze records, check for common errors, and prompt humans for input only when needed.
Let's walk you through how AI integrates into the coding workflow of a modern-day RCM system:
Automated Code Assignment
AI can automatically assign diagnosis and procedure codes by analyzing clinical documentation, structured data, and supporting evidence within the medical record.
Unlike basic keyword-based tools, modern AI models evaluate:
- Clinical context across the entire encounter
- Relationships between diagnoses, procedures, and medical decision-making
- Documentation elements required by coding guidelines and payer policies
This allows AI to generate codes that align not only with what was documented, but with how the care was delivered and why certain decisions were made. For high-volume encounters, automated code assignment reduces turnaround time while maintaining consistency across similar cases.
Recommended Reading: Real-world use-cases of AI in RCM workflows
Routing Complex or High-Risk Cases for Human Review
Not every encounter can (and should) be fully automated, and good AI systems are built to recognize that.
AI can score encounters based on complexity, risk, or uncertainty and automatically route specific cases to human coders for review. These may include:
- High-severity or high-dollar claims
- Encounters with ambiguous documentation
- Cases involving modifiers, trauma, or multiple specialties
By separating straightforward cases from those that require expert judgment, AI helps coding teams focus their time where it adds the most value—without slowing down the entire workflow.
Real-Time Clinical Documentation Improvement (CDI) Review
AI can identify documentation gaps before coding and billing occur.
During or immediately after an encounter, AI can flag:
- Missing specificity or incomplete diagnoses
- Unsupported levels of service
- Missing documentation for independent interpretation or risk factors
This enables real-time or near-real-time CDI feedback, reducing the need for retrospective queries and minimizing downstream denials. When clinical reasoning is captured early, coding decisions become clearer and more defensible later in the revenue cycle.
Integration With Widely Used EHRs
For AI in medical coding to be effective at scale, it must integrate seamlessly with existing systems.
Modern AI tools are designed to:
- Read encounter notes directly from the EHR
- Analyze structured and unstructured data in place
- Return codes, rationale, and flags without requiring duplicate workflows
Tight integration ensures that AI fits into established coding and documentation processes rather than forcing teams to adopt parallel systems. This is especially important for maintaining adoption, accuracy, and audit readiness.
What Are the Benefits of Using AI in Medical Coding
AI in medical coding delivers its most measurable value where small gaps within the RCM process tend to happen. Think documentation errors, inconsistent interpretation, or missing clinical justification, all of which can compound into claim denials once the claim is processed.
AI can help reduce the conditions that lead to denials in the first place.
Here are the benefits AI medical coding offers:
Fewer Denials From Incomplete or Unsupported Coding
One of the most common denial reasons is a lack of medical necessity or insufficient documentation to support billed services.
AI systems can evaluate whether:
- Each CPT or HCPCS code is supported by documented diagnoses
- The clinical story aligns with the level of service billed
- Required documentation elements are present before claims are submitted
Consistent Application of Coding Guidelines and Payer Rules
Human coding variability is a hidden driver of denials.
Two coders may reasonably interpret the same chart differently, especially under time pressure or high volume. Payers, however, expect consistency.
AI applies:
- Coding guidelines uniformly
- Payer-specific rules consistently
- The same logic across similar encounters, every time
Earlier Detection of Documentation Gaps That Lead to Denials
Many denials are preventable but only become visible after the claim is rejected.
AI enables earlier intervention by flagging:
- Missing specificity
- Implied but undocumented conditions
- Procedures without a clear rationale
- Conflicts between multiple note authors
.webp)
Better Use of Human Review Where Denial Risk Is Highest
Not every encounter carries the same denial risk.
AI can identify and route:
- High-dollar claims
- High-complexity encounters
- Charts with ambiguous documentation
Real-World Use Case of AI in Medical Coding
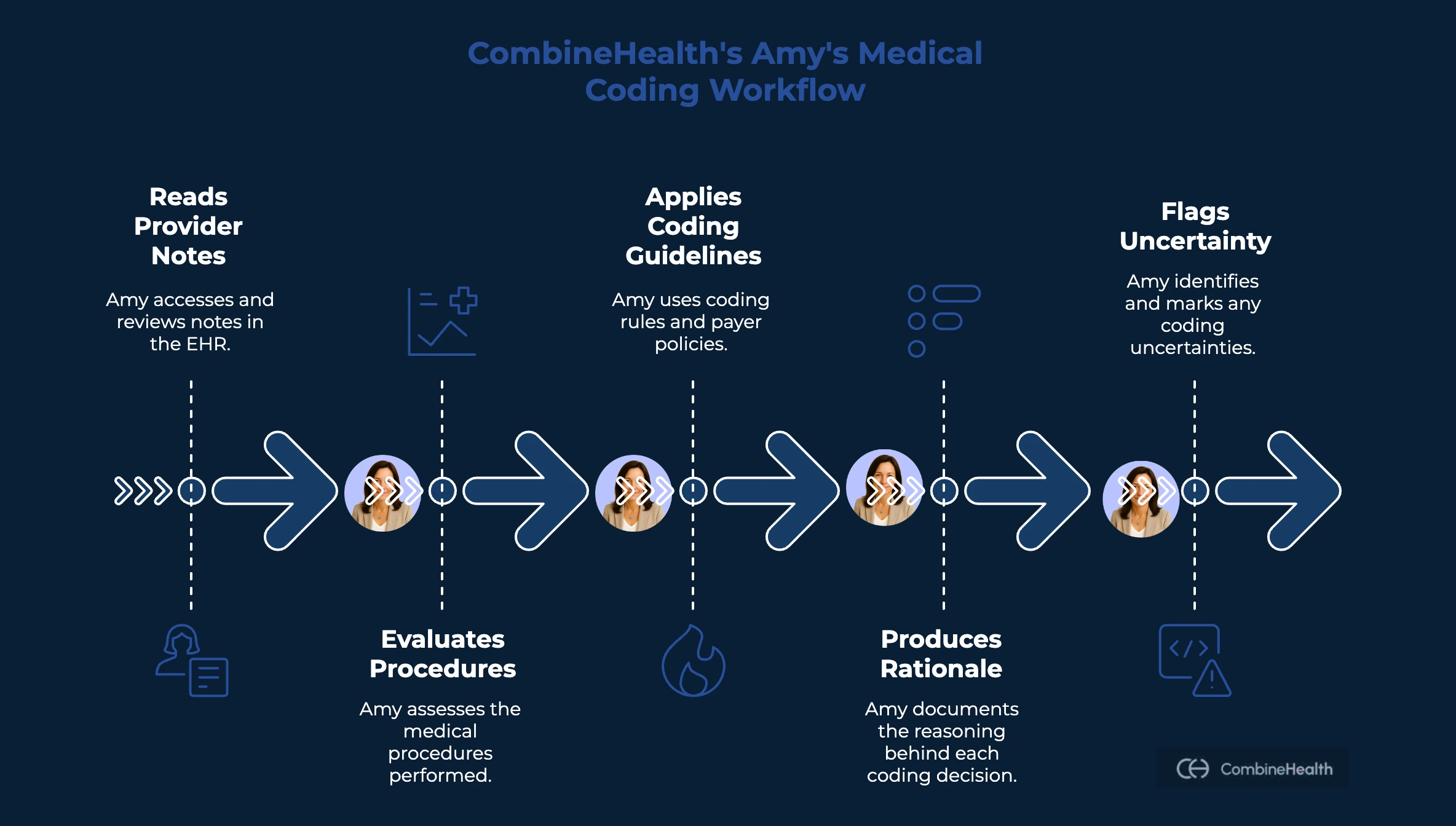
To understand how AI in medical coding works beyond theory, it helps to look at how it’s applied inside real revenue cycle workflows. At CombineHealth, medical coding automation is built around a simple principle: codes should reflect not just what was documented, but the clinical reasoning that justified the care.
That principle is operationalized through Amy, CombineHealth’s AI medical coding agent, which supports coding, auditing, and CDI across multiple specialties.
How CombineHealth's Amy AI Works
Amy is designed to work the way experienced medical coders do, by reasoning through the encounter, not scanning for keywords.
Amy's workflow:
- Reads provider-authored notes directly from the EHR
- Evaluates procedures performed, tests ordered, and resources used
- Applies coding guidelines and payer rules consistently
- Produces line-by-line rationale for each coding decision
- Flags uncertainty instead of guessing
Use Case: AI Medical Coding in the Emergency Department
The emergency department is one of the most challenging environments for medical coding. That's because ED encounters are:
- Primarily acute, not longitudinal
- Highly dependent on cognitive effort that may not be fully documented
- Influenced by trauma rules, imaging interpretation, and morbid conditions
- Documented under extreme time pressure, often with ambiguity or gaps
When CombineHealth engineers implemented AI-driven medical coding for an ED customer, they focused on teaching the system to recognize nuance before automation.
Step 1: Generating Billable Codes (CPT / HCPCS)
The first step is identifying what care was actually delivered.
Amy evaluates:
- Provider-authored clinical notes
- Procedures performed
- Facility resources used
- Tests ordered and independently interpreted
Rather than assuming everything mentioned is billable, Amy determines which elements reflect true patient care delivered during the encounter.
Step 2: Generating Non-Billable Codes (ICD-10)
Once billable services are identified, Amy generates ICD-10 codes to tell the clinical story that justifies those charges.
Here, Amy works from first principles:
- What symptoms did the patient present with?
- What acute conditions required intervention?
- Which chronic conditions complicated care or increased risk?
After assigning ICD-10 codes, Amy performs a second validation pass:
Does each CPT or HCPCS code have clear clinical justification within the ICD set?
Ready to Streamline Your Medical Coding Workflows?
Medical coding may not be the most exciting part of running a clinic, but it's one of the most important healthcare operations. More than just translating notes into numbers, it keeps revenue flowing and helps ensure you're getting paid for the services you delivered.
If you're looking to streamline your coding process and eliminate errors, book a demo with us to see how Amy AI can help!
FAQs
What is medical coding, and why is it important for clinics?
Medical coding is the process of turning details from patient visits into standardized codes used for insurance billing, reporting, and tracking outcomes. Accurate coding ensures clinics are reimbursed fairly and on time while reducing claim denials and administrative headaches.
What is the difference between medical billing and coding?
Medical coding translates clinical documentation into standardized codes (ICD-10, CPT, HCPCS). Medical billing uses those codes to submit claims, follow up with payers, post payments, and manage denials. Coding comes first; billing turns codes into revenue.
Will AI take over medical coding?
No. AI will automate high-volume, well-documented cases, but human coders will remain essential for complex, ambiguous, and high-risk encounters. The future is a hybrid model where AI handles scale, and humans provide oversight and judgment.
What is E/M in medical coding?
E/M (Evaluation and Management) coding captures the complexity of a patient visit based on medical decision-making, data reviewed, and patient risk. It reflects clinical reasoning, not procedures, and is one of the most judgment-driven areas of medical coding.
Which is the best AI medical coding platform?
CombineHealth’s Amy is built for autonomous medical coding with explainable reasoning, human-in-the-loop controls, and payer-aware logic—making it well-suited for reducing denials while maintaining compliance at scale.
How can coding errors impact clinic revenue?
Even small errors in medical coding may lead to denied claims, delayed payments, or extra paperwork. Consistent, correct coding is essential to avoid revenue loss and maintain efficient operations.
How is AI changing the medical coding process?
AI-powered coding tools automate much of the coding workflow by analyzing records, flagging errors, and handling routine cases. This reduces manual effort, speeds up payments, and lowers overall claim denials, leaving staff free to focus on patient care.
What types of medical codes are most commonly used?
The two main code sets are ICD codes for diagnoses and CPT codes for procedures. These standardized systems help clinics, hospitals, and insurers communicate clearly and manage billing accurately.
What can health centers do to improve their coding practices?
Health centers and hospitals should invest in regular staff training, use automation tools where possible, maintain organized electronic health records, monitor key billing metrics, and keep up to date with changing payer rules to ensure maximum accuracy and efficiency.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










