Payer Downcoding: What Is It and How Does It Impact Healthcare Revenue
Learn what payer downcoding is, why it’s rising with AI-driven audits, and how proactive RCM strategies can prevent silent revenue loss.
October 16, 2025


Key Takeaways:
• Payer downcoding happens when insurers automatically lower billed code levels, reducing legitimate reimbursement without issuing denials.
• The rise of AI-driven claim adjudication has made silent downcoding more frequent, affecting E/M services the most.
• Documentation gaps, payer-specific rules, and coder burnout are the top drivers of preventable downcoding.
• Traditional audits can’t keep up; RCM teams need real-time documentation intelligence and automated payer rule checks to stay ahead.
• Proactive prevention (not post-payment appeals) is the key to preventing downcoding before it drains revenue.
Your coding and billing teams are doing everything right. Claims go out clean, documentation checks look solid, and denials are trending down.
Then, the numbers start slipping. Payments for the same services are lower than last quarter. Reimbursement for complex visits looks off—but there are no denials, no obvious red flags. Just smaller payments and bigger variances.
That’s what happens when payers silently downcode your claims if they deem your documentation doesn’t justify the billed service. This practice is often carried out by algorithms instead of human review, but the impact is real: lost revenue, longer A/R cycles, and frustrated clinicians whose work is undervalued.
In this article, we’ll uncover what payer downcoding really means and why it happens, why it’s becoming more aggressive, and how healthcare organizations can avoid it.
What Is Downcoding in Medical Billing?
Downcoding happens when a payer reimburses a claim at a lower level of service than what was originally billed. In other words, you submit a claim for a high-complexity visit (say, CPT 99215), but the payer processes, downcodes the CPT code, and pays it as 99213.
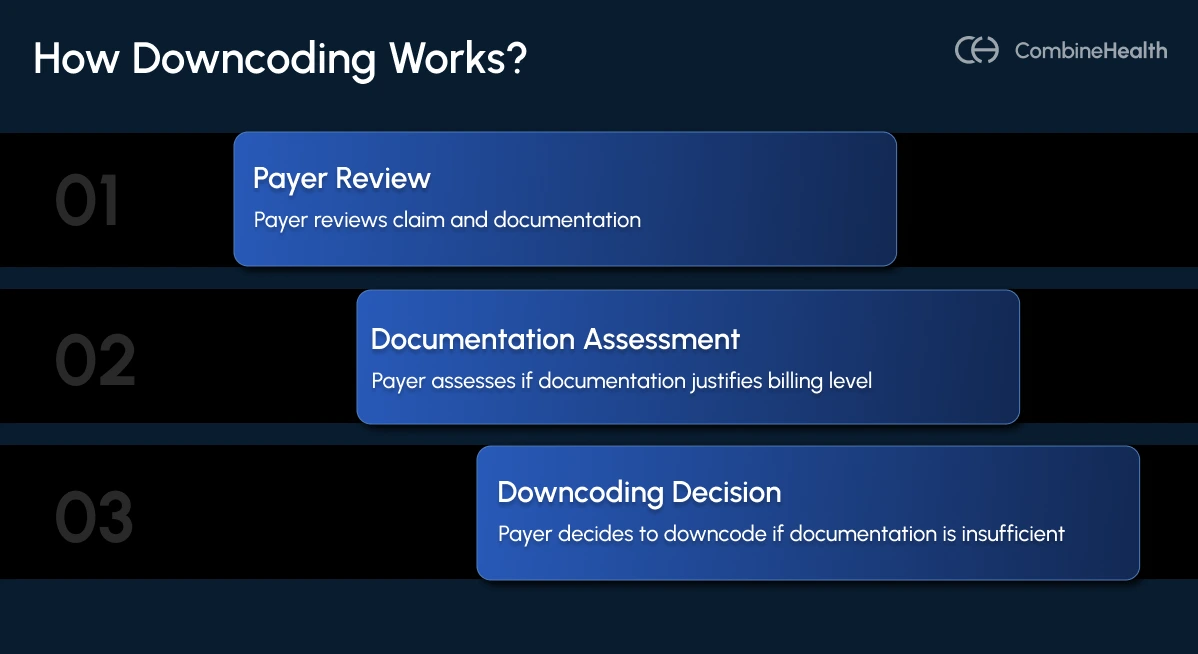
Downcoding reflects a mismatch between provider documentation and payer interpretation. When the supporting clinical documentation doesn’t fully justify the billed level, the payer’s automated system assumes the claim was “upcoded” and downgrades it.
In some cases, payers also reimburse less than the contracted rate, leading to what’s known as underpayment—a silent revenue loss that often goes undetected without proper payment validation tools.
While downcoding reduces reimbursement by lowering the code level of a billed service, underpayment occurs even when the code is accepted as submitted but the payment amount doesn’t match the contracted rate, making both equally damaging, yet harder to detect in real time.
Why Payer Downcoding Has Become So Common?
Payers have become more aggressive in recent years when it comes to flagging coding and billing errors in medical claims. Payers are now deploying tighter automation and post-payment audits, which have made payer downcoding very common. And several forces are driving this surge in automated downcoding:
- Cost Containment: AI-powered adjudication allows payers to cut claim costs in real time and protect profit margins.
- Post-2021 E/M Shifts: The rise in legitimate Level 4–5 codes after the 2021 E/M updates triggered payer scrutiny.
- Peer Comparison Algorithms: Automated benchmarking flags providers who code above peer averages, even when justified.
- Documentation Gaps: Payers often justify downcoding by claiming documentation lacks sufficient evidence for high-complexity MDM or time.

Can Downcoding Increase Reimbursements?
No, downcoding never increases reimbursements. It does the exact opposite.
From a financial standpoint, every downcoded claim represents lost revenue that the provider legitimately earned but couldn’t substantiate clearly enough on paper. For instance, if a complex patient visit (99215) is downcoded to a moderate visit (99213), the provider might lose $60–$80 per encounter.
Difference Between Upcoding and Downcoding
Although both involve discrepancies between documented care and billed codes, upcoding and downcoding sit on opposite ends of the compliance spectrum.
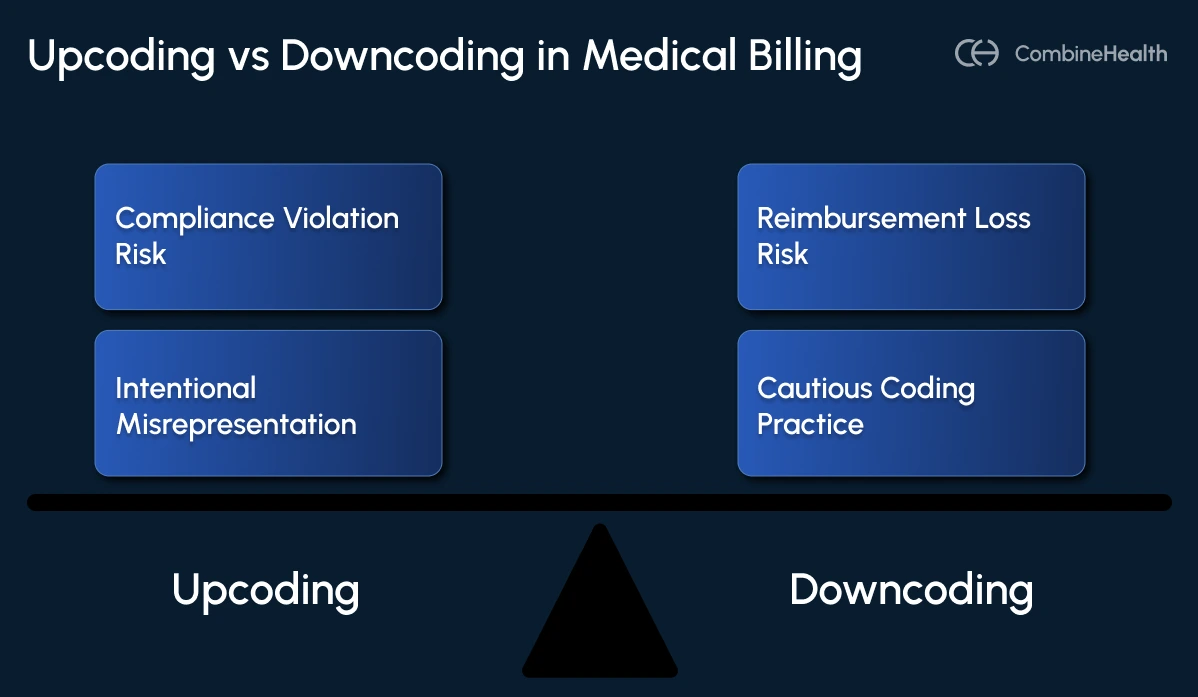
Upcoding occurs when providers bill for a service that’s more complex—or more expensive—than what was actually documented. This is often a compliance violation rather than a clerical error.
It can trigger payer audits, financial penalties, and even legal action under the False Claims Act, especially if done repeatedly or deliberately.
Downcoding, by contrast, happens when a claim is reimbursed for a lower level of service than the documentation supports. The provider loses legitimate reimbursement despite delivering the higher service level.
This can be payer-initiated (through algorithms that automatically downgrade codes) or provider-driven, when coders choose conservative codes out of caution.
Is Downcoding and Undercoding the Same?
Both downcoding and undercoding are related, but not identical.
Downcoding typically occurs during the medical coding or adjudication process, when the payer adjusts the code to a lower level.
On the other hand, undercoding usually happens on the providers’ end, i.e., when a provider or coder voluntarily assigns lower-level codes than supported by the record.
Sometimes, coders self-downcode to avoid claim denials. This typically happens when the documentation looks incomplete or ambiguous, or they’re unsure how to apply evolving E/M guidelines. And a lot of times, coder shortages, documentation fatigue, and increased workload can lead coders to such practices.
Common Causes of Downcoding
The majority of downcoded claims stem from preventable coding issues: missing documentation, unclear MDM elements, or incorrect application of payer-specific rules. Combine that with rising coder workload and shifting E/M guidelines, and you get a perfect recipe for revenue leakage.
Below are the most common reasons medical claims get downcoded, drawn from real-world RCM frustrations shared by coders, providers, and revenue cycle leaders.
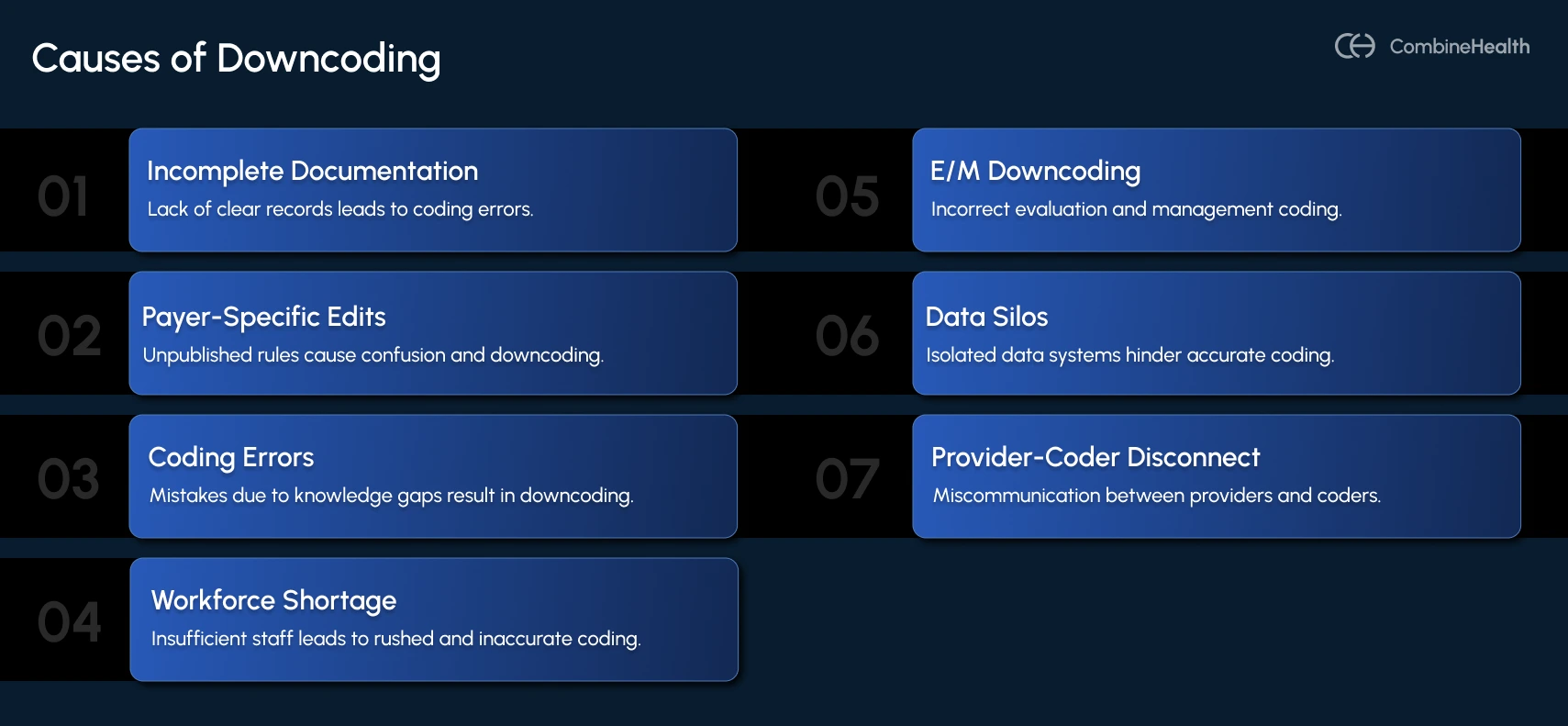
1. Incomplete or Ambiguous Documentation
When key details like time spent, medical decision-making (MDM), or exam elements are missing, payers automatically assume the encounter was less complex than billed.
In this case, a claim may be downcoded because of these reasons:
- No explicit statement of the total time spent with the patient
- Missing or vague MDM rationale (e.g., “labs reviewed” without linking findings to the final decision)
- Absence of risk assessment or the number of problems addressed
2. Payer-Specific Edits and Unpublished Rules
Even when providers submit claims using accurate CPT and ICD-10 codes, many payers apply proprietary edits and internal algorithms that override standard coding logic. These edits often stem from payer-specific policies that are not publicly available.
This problem has grown more pronounced with the rise of AI-driven claims adjudication systems, now widely used by commercial payers. Major insurers like Cigna and Aetna have adopted automated tools that reassign E/M codes based on algorithmic “medical necessity” assessments rather than full clinical review.
For example, Cigna’s Evaluation and Management Coding Accuracy policy allows automatic downcoding of higher-level visits when its system determines the documentation doesn’t support the billed level—often without examining the actual medical record.
3. Coding Errors And Knowledge Gap
A large share of downcoding originates from human error and gaps in coding expertise. When coding teams aren’t fully aligned with the latest CPT and ICD-10 updates, or when they misunderstand how current E/M and specialty-specific rules apply, they often select lower-level codes than the documentation actually supports.
.webp)
4. Workforce Shortage
The national coder shortage continues to intensify the downcoding risk. According to MedCity News, nearly 80% of healthcare organizations report turnover rates between 11% and 40% in their revenue cycle departments—a level that has left many teams struggling to keep up with growing claim volumes.
So, how does that trigger downcoding? Understaffed coders are forced to prioritize speed over accuracy, often defaulting to lower-level codes to avoid denials or compliance issues.
5. E/M Downcoding
E/M services (office visits, consultations, and patient encounters) remain the most frequent targets for payer downcoding. These encounters rely on clinical documentation that supports either medical decision-making (MDM) or total time, both of which involve subjective interpretation. That subjectivity makes E/M claims particularly vulnerable to payer algorithms and audits.
The 2021 E/M coding updates, designed to simplify documentation, also created new gray areas. By allowing coding based on MDM or total time, the rule change opened opportunities for fairer reimbursement but simultaneously increased payer scrutiny.
Now, payers are often seeing downcoding:
- Level 4 visits (CPT 99214) to Level 3 (CPT 99213), often citing “insufficient documentation,” leading to an average revenue loss of around $45 per encounter.
- Level 5 visits (CPT 99215) when MDM details or time tracking are incomplete.
- New patient visits (CPT 99202–99205) through automated “medical necessity” checks that rarely involve full record review.
6. Data Silos and Workflow Disconnects
Many downcodes aren’t due to clinical documentation at all. They stem from disconnected systems that can’t keep up with EHR upgrades or integrate RCM workflows effectively.
So, when data fails to transfer correctly between EHRs, billing software, and clearinghouses, crucial details such as modifiers or secondary diagnoses are lost.
7. Provider–Coder Disconnect
Inconsistent communication between clinicians and coders also leads to downcoding. Providers document for clinical accuracy, not coding specificity, while coders rely on structured elements tied to reimbursement.
Some providers intentionally undercode to “reduce audit risk,” inadvertently setting a lower baseline that payers then use for comparison.
Specialty-Specific Downcoding Challenges
Downcoding doesn’t affect all specialties equally. High-complexity services, where documentation must capture nuanced clinical judgment, face the greatest risk.
This includes the following specialties:
Inpatient Services and DRG Downgrades
Payers frequently reclassify high-weighted DRGs such as sepsis, acute respiratory failure, and gram-negative pneumonia to lower groupings, citing missing or incomplete indicators of major complications.
These DRG downgrades can reduce payments by $3,000 to $7,000 per claim.
Cardiology: Modifier and Bundling Risks
Cardiology procedures, including catheterizations, stent placements, and diagnostic imaging, carry intricate coding and bundling rules.
Payers often downcode when modifiers like 26 or TC are omitted or when proprietary edits automatically re-bundle professional and technical components.
Surgery: Missing Details
In surgery, even a single omitted phrase can cost thousands. For example, cases with CPT 19302 (partial mastectomy with lymph-node dissection) can be reduced to 19301 (without dissection) simply because the operative note lacked explicit wording confirming the node removal.
Emergency Medicine: Time Pressure and Documentation Gaps
Emergency departments face a constant risk of downcoding due to incomplete MDM details.
Payer algorithms frequently downgrade Level 4–5 ED visits to lower levels, citing insufficient linkage between presenting problems, test interpretations, and medical decision-making.
How Major Payers Are Leading the Downcoding Trend
Several major commercial insurers have introduced automated or algorithmic review programs that adjust Evaluation and Management (E/M) codes without full medical record review.
Cigna’s “Coding Accuracy” Reviews
Cigna’s Evaluation and Management Coding Accuracy policy enables automatic downcoding of higher-level E/M services when its proprietary algorithms determine that documentation “does not support” the billed level.
Following significant pushback from medical associations and regulatory intervention by the California Department of Managed Health Care, Cigna agreed to pause implementation in California. However, the policy remains active in other states.
Aetna Downcoding Claims With Retrospective Audit and Clawback Model
Aetna relies heavily on post-payment audits to recoup revenue after claims have already been paid. Under its E/M Claim and Code Review Program, commercial plans nationwide conduct retrospective reviews targeting “overutilizers”—providers whose coding patterns trend above peer averages.
In these cases, providers initially receive full reimbursement, only to face clawbacks weeks or months later when Aetna requests documentation. Even when notes justify higher codes, practices often face long delays and administrative burden to restore lost payments.
Regional Blue Cross and Humana
Regional Blue Cross Blue Shield plans and Humana have implemented similar AI-based downcoding systems, primarily targeting higher-level E/M visits, telehealth services, and split/shared visits.
These models automatically flag claims that exceed payer-defined thresholds for complexity or time and reassign them to lower-level codes pending provider appeal.
Why Traditional Coding Checks Aren’t Enough Anymore
For years, healthcare organizations have relied on manual audits, random chart reviews, and Computer-Assisted Coding (CAC) systems to ensure coding accuracy. While these methods catch surface-level errors, they simply can’t keep up with today’s payers’ speed, sophistication, and automation.
Here’s why the old approach falls short:
- Manual audits cover too little, too late: Most teams can review only 5–10% of charts post-submission, leaving systemic errors—and payer downcoding patterns—undetected until denials start piling up.
- CAC tools stop at keyword matching: Older systems rely on text extraction, not true understanding. They can’t interpret medical decision-making, payer logic, or real-time policy updates.
- Payer algorithms evolve faster than compliance teams: Payers now use AI to scan and adjust thousands of claims per second. Human teams relying on static coding rules simply can’t match that pace.
- Documentation feedback loops are missing: Traditional workflows don’t alert providers when their notes risk a downgrade, allowing the same documentation gaps to repeat.
- Cross-system data silos persist: Disconnected EHR, billing, and clearinghouse systems create mismatched data—one of the top contributors to preventable downcoding.
Steps to Take To Avoid Downcoding As A Healthcare RCM Leader
For RCM leaders, the goal is not only to catch downgrades after the fact but to build a revenue cycle that prevents them from happening in the first place.
1. Strengthen Clinical Documentation and Coding
Accurate coding starts with complete and defensible documentation. Gaps in medical decision-making (MDM) or time tracking are the top triggers for payer downgrades.
- Capture full MDM details—problem complexity, data reviewed, and risk level.
- Record exact minutes for time-based E/M codes; avoid vague phrasing like “lengthy visit.”
- Use precise ICD-10 codes and avoid “unspecified” diagnoses that trigger edits.
2. Educate Providers and Coders on Payer Requirements
Your team can’t defend against what they don’t know. Continuous payer education is critical to staying ahead of evolving AI-driven edits.
- Train staff on downcoding policies from Cigna, Aetna, and UnitedHealthcare.
- Share audit and appeal findings to highlight documentation improvement areas.
- Encourage coders to question ambiguous notes rather than default to lower codes
3. Benchmark and Monitor Claim Patterns
Downcoding often hides in the data. Benchmarking helps you catch outlier patterns before payers do.
- Compare E/M utilization rates to national and payer benchmarks.
- Identify providers or codes frequently targeted for adjustments.
- Track downcoding by payer, code, and location to spot recurring issues.
4. Keep Up With Payer Automation and Leverage AI
Manual reviews can’t keep up with payer automation. Modern RCM teams need tools that flag risk early and validate accuracy automatically.
- Adopt AI-driven coding and claim review tools to detect potential downgrades pre-submission.
- Automate documentation checks for missing MDM or modifier details.
- Use analytics dashboards to monitor payer trends in real time.
5. Streamline Appeals
Even with prevention, payer downcoding will happen—speed and precision in appeals make the difference.
- Appeal every unjustified downgrade with full documentation and CPT/AMA references.
- Automate appeal packet creation and submission to reduce manual workload.
- Track success rates and payer turnaround times to refine your strategy.
Prevent Payer Downcoding With Proactive Intelligence, Not Reactive Audits
Downcoding usually happens when your RCM workflow is reactive—documentation checks happening after submission, coders working in silos, and denials getting appealed once the ERAs are received.
To stop revenue erosion, healthcare organizations need proactive intelligence that detects risk before it turns into lost reimbursement. It means replacing manual audits with systems that understand how payers think and can defend every claim automatically.
That’s where CombineHealth’s AI-driven RCM technology makes the difference.
Our AI Agents help you:
- Catch documentation gaps at the point of care
- Validate codes against payer logic in real time
- Close the loop between clinical, coding, and billing teams
The result: fewer adjustments, faster collections, and confidence that every claim is paid at its rightful value.
Want to see how our AI Agents can help you prevent downcoding? Book a demo!
FAQs
Is downcoding illegal?
Downcoding isn’t inherently illegal, but it can become noncompliant if a payer reduces code levels without medical record review or violates contract terms. Providers can challenge such actions when documentation fully supports the billed level.
How to downcode an office visit?
Downcoding an office visit means billing a lower-level E/M code than supported by documentation, often due to simpler medical decision-making or shorter time spent. Though this aligns charges with the service provided, providers should avoid intentional downcoding, as it risks lost revenue, inaccurate records, and compliance issues.
There’s just one way around this: Always code accurately!
Does payer downcoding happen automatically?
Yes. Many payers now use AI-based adjudication systems that automatically reassign CPT codes based on internal algorithms. These models analyze documentation patterns, diagnosis-code pairings, or time fields and often downgrade services without human review.
Does payer downcoding happen without denial notices?
Often, yes. Payers frequently downcode claims silently—adjusting the payment rather than issuing a formal denial. The change appears as a “code correction” or “payment adjustment” on the remittance advice, making it easy for providers to miss.
Can downcoding be appealed successfully?
Yes. Providers can appeal payer downcoding decisions by submitting complete medical records and citing AMA CPT and CMS documentation guidelines. Clear MDM rationale and time tracking often lead to successful reversals when the payer’s downgrade wasn’t supported by policy.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










