Medical Coding for Emergency Rooms: All You Need to Know
Learn how emergency room medical coding works, why accuracy is critical for care and reimbursement, and how AI supports overburdened ER teams.
July 11, 2025


Key Takeaways:
• Emergency room coding is high-stakes, where every missed or incorrect code can cost thousands in lost revenue or trigger payer audits.
• Each ER type (from trauma centers to pediatric ERs) has distinct documentation and coding nuances that impact billing.
• Real-time AI coding support helps emergency teams stay compliant, fast, and accurate, even under extreme clinical pressure.
• AI agents like Amy, Deborah, and Marc streamline coding, denial appeals, and multi-payer billing in an ER setting.
When you think of emergency rooms (ERs), you probably envision flashing monitors, frantic footsteps, and doctors making split-second decisions to save lives. That’s actually on point.
But behind every patient encounter is a crucial administrative engine at play: medical coding for emergency rooms. With over 140 million ER visits annually across more than 6,000 facilities in the U.S.[1], there’s a lot of data flowing through an emergency department (ED). And every single patient visit must be coded with razor-sharp accuracy.
That’s because ERs run in tight margins, operating 24/7, fully staffed, and handling everything from minor injuries to major treatments. Even missing the code for a 3-hour critical care treatment could mean losing thousands of dollars. Beyond reimbursements, these codes also affect quality reporting, trauma registries, public health data, and hospital planning.
To help you understand medical coding for ER, this guide will break it down into digestible sections:
- The different types of ERs
- Common emergency scenarios and their associated codes
- How AI is stepping in to streamline the ER medical coding process
What Is Medical Coding for Emergency Rooms?
Emergency rooms medical coding involves translating each patient’s ER visit into standardized codes before adding it to clinical records and billing.
In an emergency department (ED), medical coding is mostly done by in-house or external coding specialists who review the physician’s ED chart after the patient is discharged. They examine details like history, exam findings, test results, diagnoses, and procedures documented to determine the specific codes that apply to the case.
Here’s how the coding process typically works:
- Picking the ICD-10-CM diagnosis codes matching the physician’s final diagnosis (or presenting symptoms if no definitive diagnosis yet)
- Adding additional codes for any complicating conditions or external causes of injury
- Assigning CPT codes for all procedures performed (like imaging studies, laceration repairs, CPR, etc.)
- Adding an evaluation and management (E/M) code representing the overall visit level
Want to hear about how technology is reshaping frontline care from a veteran with decades of healthcare expertise?
Tune in to this podcast: The role of AI in ER
What Are The Different Types of Emergency Rooms?
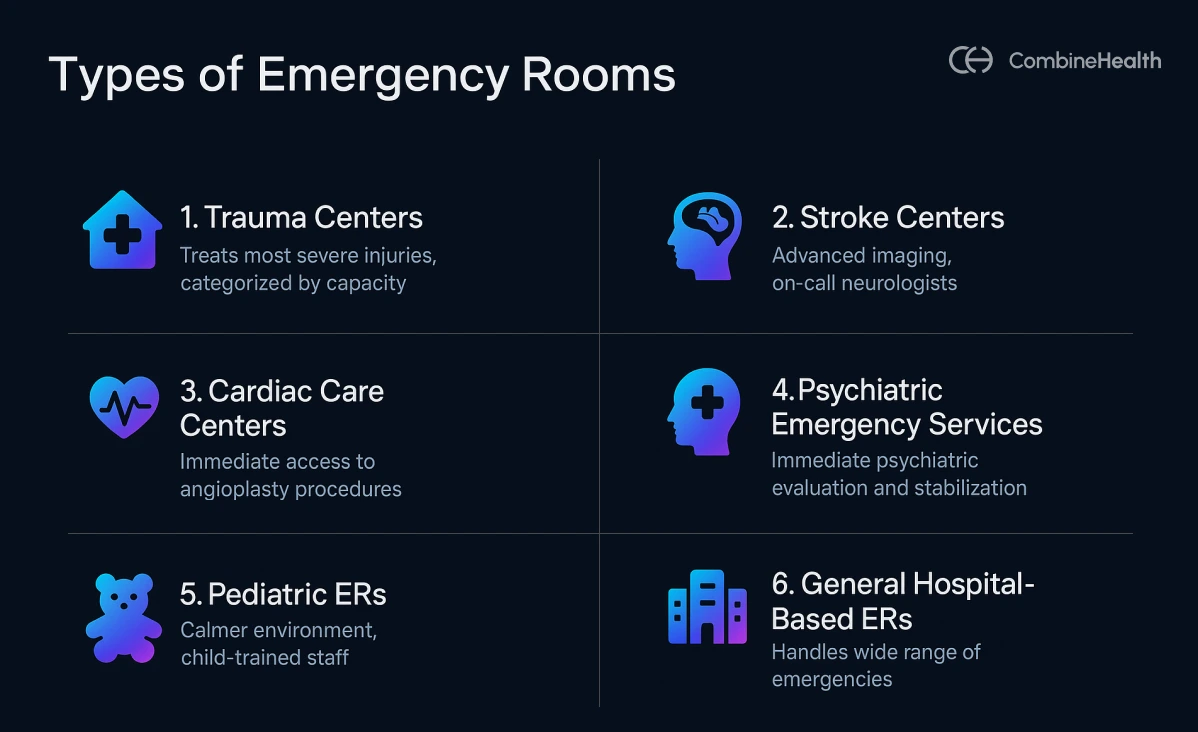
Not all ERs are the same. Each type serves different needs, and each comes with its own coding requirements.
General Hospital-Based ERs
These are found in most acute-care hospitals and handle a wide range of emergencies. They bill under the hospital's provider number, meaning the hospital will charge a facility fee for the ED visit in addition to the physician’s professional fees.
To bill to insurance, the hospitals need to submit the UB-04 claim form, filling out details for facility fee accounting for:
- The use of space
- Staff equipment
- Medical supplies
The physicians bill CPT 99281–99285 for their evaluation & management, while the hospital bills a corresponding facility code (often also 99281–99285 or a Medicare G-code) based on the resources used for the case.
Keep in mind that the coding should capture all services used for treatments, procedures, and medications, while also assigning a facility E/M level based on resource intensity.
Example:
If a patient needed IV fluids, multiple labs, and a CT scan, the facility component would likely be coded at a higher level than a simple visit with one bandage.
Pediatric ERs
Designed for children and teens (often within a children's hospital or a separate pediatric section), these ERs use specialized child-size equipment and pediatric-trained staff. The environment is usually calmer and more supportive for young patients and their families.
Pediatric ERs use the same code sets as general ERs, but the E/M level depends on the pediatric conditions (e.g., croup, bronchiolitis, playground injuries) and weight-based drug dosing.
The documentation in pediatric cases must include details like patient weight (for medication coding) and growth charts if relevant. Also, pediatric ERs might be more likely to use moderate sedation codes when doing procedures on kids (to keep them still and calm), so coders need to capture those when documented.
Example:
A 4-year-old arrives with a 2.5 cm forehead cut from a playground fall. The provider uses moderate sedation to calm the child before stitching the wound.
Codes used:
ICD-10: S01.81XA – Forehead laceration, initial encounter
CPT: 12011 – Simple facial wound repair (2.5 cm)
CPT: 99151 – Moderate sedation, <5 years
E/M: 99283 or 99284, depending on MDM
Trauma Centers
Trauma centers treat the most critical, life-threatening injuries—think multi-system trauma, gunshot wounds, or high-speed car crashes. They’re often a part of large hospitals or academic medical centers and are categorized from level I to level IV based on their capabilities.
Trauma cases generally generate intensive coding. They often involve:
- Multiple ICD-10-CM codes to describe each injury site (often S-codes)
- External cause codes to explain how the injury happened
- A slew of CPT and HCPCS codes for emergency procedures (like intubations, chest tubes, central lines, emergency surgeries, and blood transfusions)
Stroke Centers
Some hospitals have specialized stroke centers within or alongside the ED. These centers focus on the rapid evaluation and treatment of strokes.
Example:
For ischemic strokes = tPA (alteplase) or perform mechanical thrombectomy
For hemorrhagic strokes = rapid neurosurgical interventions
These ERs are equipped with advanced imaging tools and on-call neurologists. Timely stroke care here can mean the difference between recovery and long-term disability.
Stroke cases that are critically ill (e.g., requiring continuous neurological monitoring, blood pressure management in an ICU setting initiated in the ED) may qualify for critical care coding as part of the ED stay
Cardiac Care Centers
Focused on heart emergencies like heart attacks, these ERs have immediate access to procedures like angioplasty. Quick action here saves lives, and proper coding helps ensure that lifesaving care gets reimbursed.
Common ED procedures for cardiac events include:
- CPR if the patient had cardiac arrest (code is CPT 92950)
- Defibrillation (typically included in the CPR code if performed during the arrest)
- 12-lead EKGs (CPT 93005 for the tracing and 93010 for interpretation)
If the patient goes to the cath lab directly from the ED, those interventions, like percutaneous coronary intervention (CPT codes 92928), are usually billed by the cardiologist and not as part of the ED services. However, the ED coder should still code any stabilization procedures the ED team did (e.g., intubation, central line placement for cardiogenic shock, etc.).
Psychiatric Emergency Services
Some hospitals (especially large urban ones) have dedicated Psychiatric ERs or PES (Psychiatric Emergency Service) units. These are designed for mental health crises, treating patients with severe anxiety, psychosis, suicidal ideation, overdose without medical complications, etc.
Coding psychiatric ER visits requires capturing the psychiatric diagnoses, i.e., the ICD-10-CM codes in the F01–F99 range for mental disorders.
Example:
A 28-year-old presents to the ER with suicidal thoughts and a history of depression. A mental health clinician performs a full psychiatric evaluation, and the patient is admitted voluntarily.
Codes used:
F32.9 = Major depressive disorder
R45.851 = Suicidal ideation
CPT 90791 = Psychiatric diagnostic evaluation
Stand-Alone Emergency Rooms (FSEDs)
These are ER facilities not attached to a hospital. They provide emergency care in communities that may be far from hospitals or in suburban areas to offload hospital ER volume.
From a coding and billing perspective, stand-alone ERs usually bill as their own entity. This means they charge professional fees and facility fees for every service, much like a hospital ER, but since they’re not under a hospital’s license, they generate separate claims.
Coders in a freestanding ER have to code all services provided on-site, which might include things like infusions, injections, X-rays, CT scans (if the facility has a CT scanner), etc., similar to hospital outpatient coding.
Common ER Scenarios and Their Codes
In an ED, the E/M CPT codes range from 99281 to 99285 and are based not on time, but on the medical decision-making (MDM) involved[2]. Here’s an overview of what each code reflects:
ED visits span a wide range of clinical scenarios, each with distinct diagnoses, procedures, and documentation needs. In the sections below, you’ll find common ER case types, their associated diagnosis (ICD-10-CM) and procedure (CPT/HCPCS) codes to support accurate billing.
Trauma and Injuries
- Accidents & Physical Trauma: ICD-10 Sxx or Vxx codes; CPT codes for X-rays (e.g., 71020) or fracture care (e.g., 27750).
- Burns: ICD-10 T20–T25; CPT 16020 for burn dressings.
- Lacerations: ICD-10 S01–S11; CPT codes 12001–12018 for wound closure.
Medical Emergencies
- Cardiac Events: ICD-10 I21 for heart attacks; CPT 92950 (CPR), 93005 (ECG).
- Respiratory Distress: ICD-10 J44/J45; CPT 94640 for breathing treatments.
- Neurological Symptoms: ICD-10 I63 for stroke; CPT 99291 for critical care.
Acute Illnesses and Infections
- Flu & COVID-19: ICD-10 J10.1 or B97.29; CPT 87804 for rapid flu tests.
- GI Issues: ICD-10 K35 for appendicitis; CPT 74177 for abdominal CT scans.
- Kidney/Urological Issues: ICD-10 N20.0 for kidney stones; CPT 50020 for drainage procedures.
Psychiatric and Substance-Related Crises
- Mental Health: ICD-10 F32 for depression; CPT 90791 for psychiatric evaluation.
- Substance Abuse: ICD-10 T40.1 for overdose; CPT 99213 for moderate-level visits.
Critical Care E/M Codes in the ER
Some ER patients need immediate, intensive care to avoid life-threatening deterioration. These cases are coded under critical care E/M codes:
- 99291: First 30–74 minutes of critical care.
- 99292: Each additional 30 minutes beyond the initial.

What Are The Challenges of Coding for ER?
In a typical ER environment, medical coders aren’t just chasing accuracy. They’re also balancing speed, consistency, and compliance under intense pressure.
Here are some problems most ER coders usually face:
- High volume of cases: ER coding must be fast and accurate, which leads to burnout among coders and clinicians alike.
- High skills demand: Coders face a wide variety of complex cases every day: head trauma, chest pain, broken bones, sepsis, stroke. Each case demands precise code selection, often across multiple body systems.
- Frequent CDI gaps: ER physicians are also overworked, juggling multiple patients at once. They often have limited time for documentation, which creates clinical documentation integrity (CDI) gaps.
- High risk of denials: Physicians can’t always wait for official test results. So they often perform independent interpretation, reviewing CTs or EKGs themselves and making critical decisions on the fly. Limited patient history, split-second decisions, and defensive medicine practices can all lead to aggressive documentation.
- Changing payer guidelines: Coding rules and billing requirements are frequently updated by CMS and private insurers. They can be difficult to keep up with, and coders need to educate themselves on the current guidelines constantly.

And mistakes in an ED can be costly. Every missed code, vague note, or unsupported level of service puts revenue and compliance at risk.
Example:
Incorrect or missing code for a 3-hour critical care service could mean losing thousands in reimbursement, while over-coding a simple visit can trigger audits, denials, or even fraud investigations.
If a coder omits a key diagnosis or procedure, the hospital may never get paid for services rendered. On the flip side, upcoding can trigger overpayments, repayments, and serious penalties under fraud and abuse regulations.
How AI Simplifies Emergency Room Medical Coding
AI’s role in ER medical coding is to amplify and support your coding efforts, not replace clinical coding expertise.
AI takes care of routine reviews and flags issues in real time, easing the load on busy coders and doctors. This way, coders can focus on complex cases and improve documentation, without adding to burnout or slowing down the ER.
CombineHealth’s AI agents Amy, Deborah, and Marc help you fix your coding discrepancies in real-time and handle large volumes of data at once. Here’s how the trio assists an ER team:
1. Amy: The Coding Assistant
Amy is built to handle the high volume and clinical complexity of emergency department cases. She reviews clinical notes, test results, diagnoses, and procedures in real time and:
- Assigns accurate ICD-10 and CPT codes, even for complex, multi-system presentations like trauma or cardiac events.
- Explains E/M code choices, breaking down MDM (medical decision-making) components like problem complexity, data reviewed, and risk.
- Flags missing CDI gaps, such as chronic conditions, patient weight, or drug administration details.
2. Deborah: The Denial Expert
Emergency physicians often work with limited patient history and tight timelines, leading to aggressive documentation and a high risk of payer denials. That’s where Deborah comes in.
- She prepares medical necessity appeals when payers question high-level E/M codes or critical care claims.
- She builds appeals based on clinical evidence that Amy surfaced and cites the medical urgency and decision-making rationale.
3. Marc: The AI Billing Engine
Emergency rooms often deal with patients covered by multiple insurers, creating billing chaos. Marc manages this seamlessly by:
- Handling end-to-end billing, from claim generation to submission, tracking, and follow-up.
- Identifying and routing claims to the correct primary payer, minimizing rejections due to coordination of benefits issues.
- Ensuring timely follow-ups and resubmissions, maximizing collections without manual intervention.
Optimize ER Coding With AI On Your Side
Emergency room visits are among the most complex to code, and every detail matters. By understanding the types of ERs, common scenarios, and how coding is structured, you can ensure accurate billing and better patient record-keeping.
With AI tools like Amy, coding becomes less stressful and more reliable, helping teams deliver better care without sacrificing administrative precision.
Need help improving your ER coding efficiency?
Contact us to learn how AI can support your emergency department today.
References
[1]PubMed. https://pmc.ncbi.nlm.nih.gov/articles/PMC11368583, sourced 11 July, 2025
[2]ND. https://www.bcbsnd.com/providers/policies-precertification/reimbursement-policy/coding-guidelines-for-emergency-department, sourced 11 July, 2025
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










