Independent Interpretation Explained: Why It Matters For Your CDI and How To Get It Right
Independent interpretation is the key to accurate coding and stronger MDM. This blog explains what it is, why it matters, and how getting it right can protect your revenue and clean up your CDI.
July 16, 2025


Key Takeaways:
• Independent interpretation is an important MDM data element.
• Under the 2021 E/M guidelines, personally interpreting a test (without billing for it) qualifies as Category 2 data and can help elevate a visit's MDM level.
• A properly documented interpretation can bump a visit from low to moderate or moderate to high MDM, leading to more accurate reimbursement.
• Missed interpretations = missed revenue. Coding a visit one level too low (e.g., 99213 vs. 99214) can cost $30–$40 per encounter. Over time, that adds up to significant leakage.
• ED providers often make decisions before official reports are available. Documenting independent reads (e.g., of CT or EKG) supports higher E/M levels like 99285.
Think about the last time you reviewed a provider’s clinical documentation and something just didn’t add up.
Maybe they noted “chest X-ray reviewed,” but didn’t specify what they observed.
Maybe they quoted the radiologist’s report as their finding.
Maybe the MDM level felt too low for how complex the visit actually was.
One of our sources recently told us that 40% of their CDI issues stemmed from one specific cause: Independent Interpretation (or rather, the lack of it)[1].
This is why, when the Centers for Medicare & Medicaid Services (CMS) and the American Medical Association (AMA) overhauled office/outpatient E/M coding in 2021, they made independent interpretation a non-negotiable step in the E/M coding process. This shift was meant to simplify documentation, reduce administrative overhead, and reward real decision-making. But it only works if your teams know how (and when) to use it.
Let’s look at what independent interpretation even means, why it matters, and how executing it well can help you reduce denials and strengthen your CDI program.
What Is Independent Interpretation?
Independent Interpretation is a critical component of Evaluation and Management (E/M) that requires the treating physician to personally review and interpret the original test data from a diagnostic test performed by another healthcare professional.
But this doesn’t mean rubber-stamping a radiologist’s or cardiologist’s report. Rather than relying solely on a specialist’s findings, the physician must document their own interpretation in the medical record.
According to the AMA, independent interpretation applies only when the physician is interpreting a test that has a corresponding CPT code, and for which an interpretation or report is customary[2]. Also, the physician must not bill separately for that interpretation.
Independent Interpretation is more than just a checkbox in the E/M process. It demonstrates cognitive effort, showing you're not just accepting someone else’s conclusions, but actively using your clinical expertise to guide patient care.
This added complexity can elevate the MDM level of an encounter, which in turn supports a higher-level, more accurate E/M code.

Important E/M Guidelines About Independent Interpretation
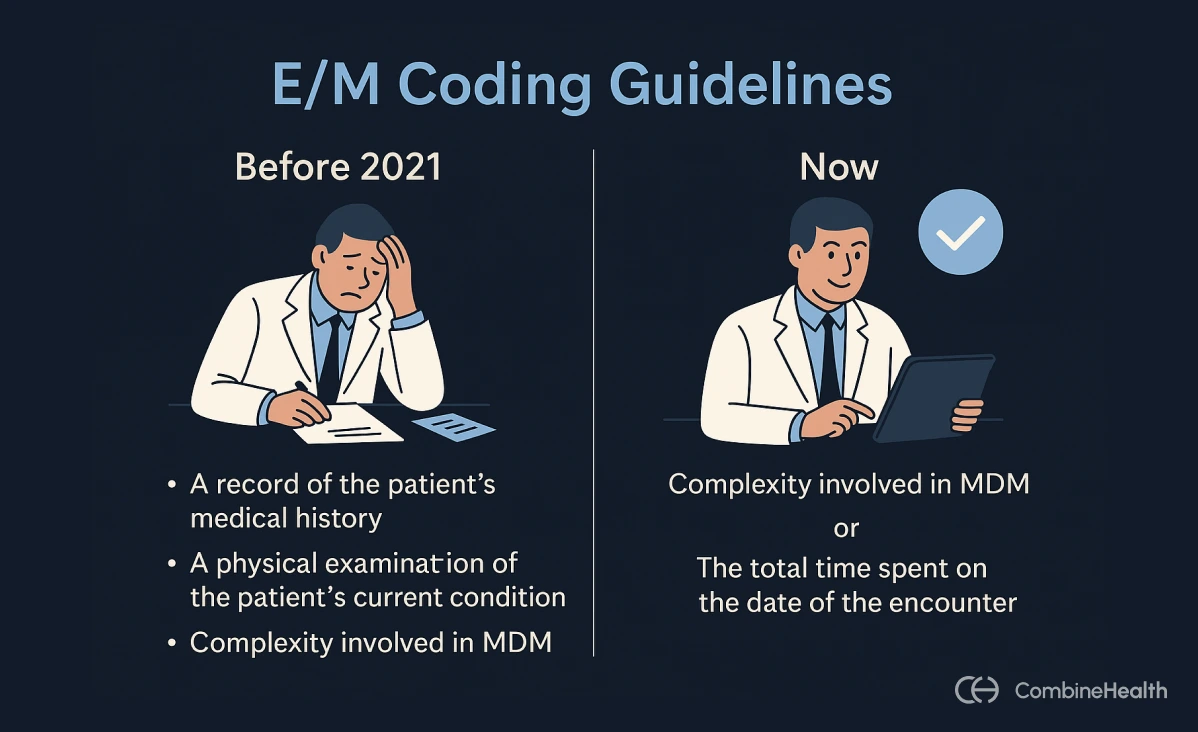
Before 2021, providers had to carefully document three components to justify an office or outpatient E/M code:
- A record of the patient’s medical history
- A physical examination of the patient’s current condition
- A clinical assessment of the complexity involved in the provider’s decision-making process (MDM)
Exception: If more than 50% of the visit was spent on counseling or coordinating care, then you could use time as a component to select the code instead.
In practice, this meant a lot of clinical notes were overloaded with templated histories and exams, not necessarily because they were clinically relevant, but because coding required it. The documentation process was often time-consuming, outdated, and a poor reflection of how care was actually delivered.
What Changed After The New 2021 E/M Guidelines?
Starting in 2021, the Centers for Medicare & Medicaid Services (CMS) and the American Medical Association (AMA) introduced new rules to simplify how providers code office and outpatient visits[3]. The goal was to reduce documentation burden and make coding better reflect actual clinical work.
So, what changed?
Instead of requiring providers to document history, physical exam, and MDM, the new rules allow code selection based on either of these two components:
- The level of MDM (straightforward, low, moderate, or high)
- The total time spent on the date of the encounter
Note: History and physical exam are still part of the visit, but they’re only needed if they’re medically appropriate. They don’t count toward the code selection anymore.
If you're coding based on time, you now include the total time spent on that calendar date. That means everything the provider does related to the visit, not just face-to-face time. This can include:
- Reviewing records and test results
- Reviewing history
- Ordering labs or other tests
- Documenting the encounter
But first, What Are MDM Levels?
MDM reflects the thought process and complexity behind the care you provide. It’s about what decisions you make, what data you analyze, and what risks you manage during the encounter.
There are four MDM levels used for office and outpatient E/M coding under the 2021 guidelines:
Each MDM level is based on three elements:
- Problem complexity: Number and complexity of problems addressed
- Data complexity: Amount and/or complexity of data to be reviewed and analyzed
- Risk complexity: Risk of complications, morbidity, or mortality from patient management
To reach a specific MDM level, two out of these three elements must meet or exceed the criteria for that level.
Example:
For the patient with uncontrolled diabetes and hypertension (from the table above), the provider determines the MDM level as moderate by evaluating these elements:
• Multiple problems addressed: Managing two chronic, uncontrolled conditions increases the complexity of problems
• Complexity of data: The provider orders diagnostic tests, contributing to moderate data complexity
Since two of the three MDM elements (problem complexity and data complexity) meet the moderate level, this encounter qualifies as moderate MDM.
How Does Independent Interpretation Help Close CDI Gaps
There are several ways independent interpretation closes documentation gaps and benefits both patient care and the bottom line:
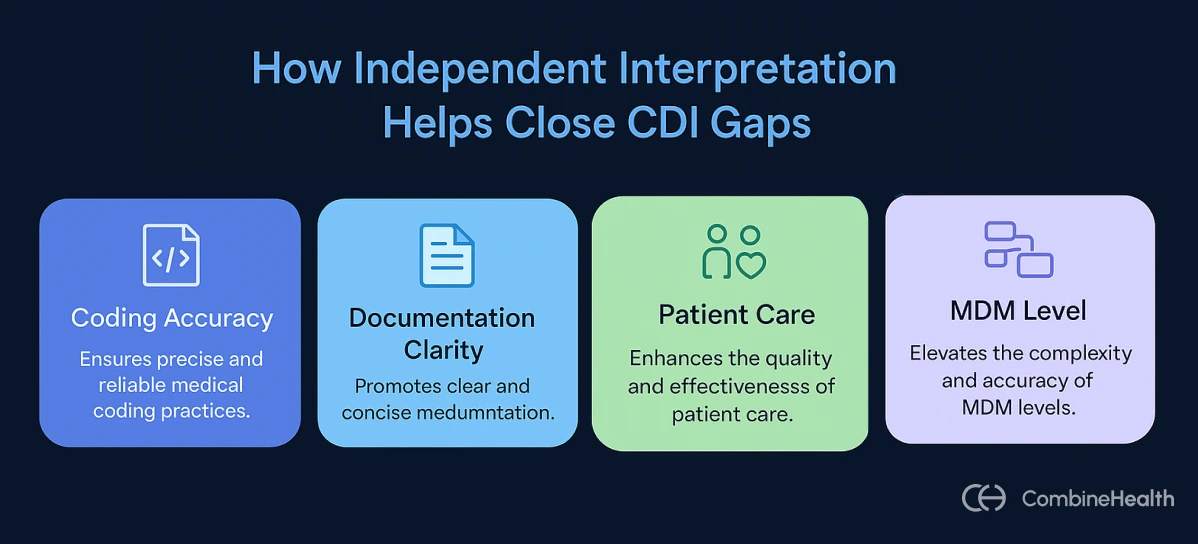
Increases Coding Accuracy
When providers document their own interpretation of raw test data (like CT images or ECG strips), they create a direct, traceable input to the MDM component of E/M coding.
That kind of documentation justifies a higher E/M code (when clinically appropriate), so the service level matches the work actually performed. Otherwise, you're doing level 4 work and getting paid like it's level 3.
For CFOs, this is low-hanging fruit.
When providers document their own interpretation of raw test data, such as CT images or ECG strips, it contributes directly to the MDM component in E/M coding. This documentation supports appropriate code level selection based on the provider’s cognitive work.
One missed level (say, coding 99213 instead of 99214) costs $30–$40 per visit, according to AAPC[4]. Multiply that by hundreds of encounters, and the financial leakage becomes obvious. Tens of thousands, gone—not because care wasn’t delivered, but because the thought process didn’t make it into the note.
Assists in Cleaner documentation
When providers explicitly note what was reviewed and what was concluded, it results in a more thorough medical record. This completeness means fewer queries from CDI specialists or payers asking for clarification.
Example:
Instead of: “X-ray reviewed”
Try saying: “Independently interpreted the X-ray, which showed no acute fracture, confirming the diagnosis of sprain.”
To meet E/M requirements, the provider’s note must include:
- A clear statement of personal review (e.g., “I personally reviewed today’s AP and lateral chest X-rays”)
- A concise statement of findings (e.g., “No acute cardiopulmonary abnormalities, no infiltrates”)
This clarity ensures that coders and CDI teams have the details they need to assign the correct level of service.
Helps Improve Patient Care
When providers interpret test results themselves, they often make more informed decisions in real time. It could be confirming outpatient treatment or ruling out a more serious condition.
It’s also a built-in safeguard. A second look often reveals what the first one missed.
Example:
A primary care doctor might personally review a patient’s chest X-ray and spot a developing pneumonia that the initial radiologist report termed as “clear”. This could help prompt an earlier treatment.
And the value doesn’t stop there. Thorough documentation of these interpretations informs the broader care team and creates continuity at follow-up. Over time, this level of rigor helps catch subtle ECG abnormalities, prevent missed fractures, and reduce diagnostic delays.
Elevates the MDM Level and Data Complexity
Independent interpretation is often the factor that elevates the MDM level for a visit from low to moderate or from moderate to high.
Under the current E/M guidelines, documenting an independent interpretation earns credit in the “Data” column of MDM[5]. In fact, it falls under Category 2 data in the MDM scoring system.
But first, let us explain what categories are under the “data” column of MDM:
- Category 1 (Tests, documents, orders, or independent historian): Ordering or reviewing tests, reviewing external notes, or getting history from an independent source.
- Category 2 (Independent interpretation of tests): Personally interpreting a test (like an ECG or MRI) that was done by someone else, without billing separately for it.
- Category 3 (Discussion of test interpretation or management): Discussing the test or patient management with another provider who’s not in your same group.
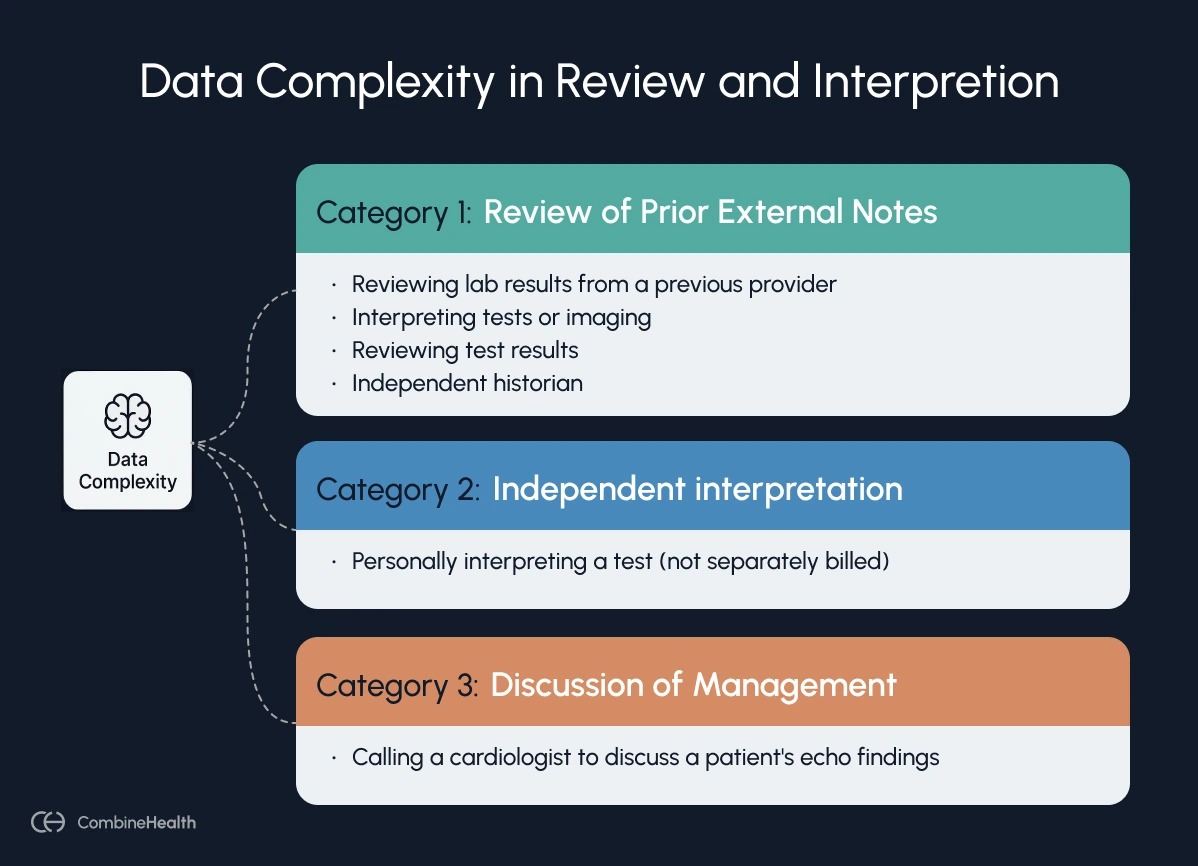
And here’s the important part: to meet moderate data complexity, you only need to meet one category. This means a single documented independent interpretation can fulfill that requirement on its own.
Example:
A patient presents with vague neurological symptoms.
The provider orders an MRI, which is officially read by radiology as normal. However, the clinician personally reviews the images, notices a subtle lesion, and documents their findings and follow-up plan. That independent interpretation contributes to high data complexity. Combined with the clinical risk, the visit could justifiably be coded as a Level 5 E/M.
By contrast, if that same interpretation wasn’t documented, the visit might only qualify for Level 4, despite the work actually done.
Independent Interpretation in the Emergency Room (ER)
As of 2023, the AMA’s updated E/M guidelines apply to Emergency Department (ED) visits, too[6]. This means ED E/M levels are now determined by MDM, just like office visits.
But why does this matter?
Emergency physicians often have to make immediate, high-stakes decisions based on imaging and test data, before a specialist’s formal report is available. Whether it’s reading a chest X-ray at 2 AM to rule out a pneumothorax or interpreting an EKG during an active MI, these real-time interpretations are part of the physician’s cognitive workload, and they should be documented.
By capturing and documenting these independent interpretations, ED providers can support higher MDM complexity and more accurate E/M coding.
Example:
An ER physician independently reviews a head CT while the radiologist’s report is still pending.
They document:
“CT brain independently reviewed – I note a small epidural hematoma, neurosurgery consulted immediately.”
This level of clinical insight and decision-making supports high MDM complexity and justifies billing 99285 instead of 99284.
What are the Documentation Requirements for Independent Interpretation?
To meet documentation guidelines for independent interpretation under current E/M rules, providers need to document the following:
- Personal review of the test: You must examine the actual image, tracing, or result yourself. That’s what makes it “independent.”
- Provider’s own interpretation: You must record their own findings or conclusions from that review in the medical record. This doesn’t have to be a full formal radiology report, but it should be more than “reviewed X-ray – OK.”
- Impact on Patient Care: It should be evident how this independent review affected your management or decision-making for the patient. The AMA’s guidelines stress that simply restating the test result isn’t enough, and you should tie it into your assessment or plan.
Some examples of acceptable documentation:
1. "Chest x-ray independently interpreted and reviewed by me; no acute cardiopulmonary abnormalities, no infiltrates, no pulmonary vascular congestion."
2. "I personally reviewed the axial and coronal cuts of the 9 July CT chest; no pulmonary embolus or consolidation is seen. Findings support outpatient treatment of bronchitis—no antibiotics, return precautions discussed."
3. "I personally reviewed the axial and coronal images from the 7 July chest CT; no pulmonary embolus or infiltrate is visible."
Example of an unacceptable interpretation:
“I personally reviewed today’s AP and lateral chest X-rays”
How Does CombineHealth Help Streamline Your CDI Process
CombineHealth’s Amy and Lia help you clean your CDI process, so you can stop chasing denials and start closing documentation gaps before they happen.
Here’s how both the AI agents work with you:
- Lia captures your clinical conversations during a patient encounter in real-time.
- Using the information she gathered, she creates EHR-ready notes.
- Amy reviews Lia’s notes, flags missing clinical indicators, vague diagnoses, or unsupported conditions.
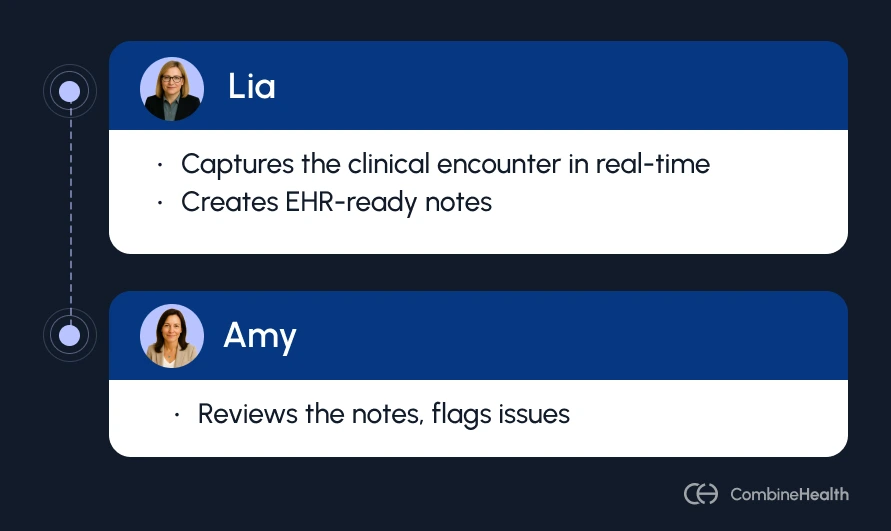
Together, they:
- Spot incomplete or vague documentation that could lead to revenue loss
- Suggest clinical evidence to justify diagnoses or procedures
- Strengthen your MDM with well-supported, higher-complexity encounters
- Help you submit the claim to payer scrutiny with confidence
Curious how Amy and Lia work behind the scenes to assist with your clinical documentation? Book a demo with us.
FAQs
What is the difference between a review and an interpretation?
A review involves the provider reading another clinician’s interpretation (for example, reading the radiologist’s report of an X-ray).
An independent interpretation, on the other hand, means the provider personally examines the original test data (like the actual X-ray image or ECG tracing) and documents their own conclusions.
This is considered a higher level of cognitive work and can be credited under the Data component of MDM, if it’s not separately billed.
What does a high MDM mean?
High MDM means the provider is managing a complex or high-risk case. It involves serious conditions, extensive data review, and decisions that carry significant risk, like starting high-risk meds or hospitalizing the patient. It supports billing the highest level E/M codes.
Who is an independent historian?
An independent historian is someone other than the patient (like a parent, caregiver, or legal guardian) who provides key medical history when the patient can’t reliably do so themselves (due to age, cognitive issues, or medical condition).
What qualifies as an independent interpretation of a test for Category 2 MDM data?
For Category 2 credit, an independent interpretation means the provider personally reviews the original test data (e.g., images, tracings, specimens) and documents their own interpretation, without billing separately for it.
The test must be one that typically includes a formal report (like an X-ray or ECG). Just reading the radiologist’s or cardiologist’s report does not qualify.
References
[1]Edelberg. https://www.edelberg.com/, sourced July 16, 2025
[2]American Medical Association. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf, sourced July 16, 2025
[3]American Academy of Professional Coders. https://www.aapc.com/resources/evaluation-management-coding-changes-2021, sourced July 16, 2025
[4]American Academy of Professional Coders. https://www.aapc.com/blog/87649-finding-the-lost-dollar, sourced July 16, 2025
[5]ID Society. https://www.idsociety.org/globalassets/idsa/clinical-practice/em-office-visit-reference-guide-01-19-2021.pdf, sourced July 16, 2025
[6]American College of Emergency Physicians. https://www.acep.org/administration/reimbursement/reimbursement-faqs/2023-ed-em-guidelines-faqs, sourced July 16, 2025
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










