Understanding Medical Decision Making in Healthcare and Why It Matters
Understand why accurate medical decision making is crucial for healthcare reimbursement and what steps are required for MDM documentation.
December 8, 2025


Key Takeaways:
• MDM is now the primary driver of E/M levels, reimbursement, and audit risk in healthcare.
• Incomplete documentation suppresses HCCs and CMI, costing organizations millions in value-based revenue.
• Clinicians already do the cognitive work; the gap is capturing their reasoning clearly and consistently in the note.
• Most MDM errors stem from cloned notes, vague data, missing SDOH impact, and undocumented independent interpretation.
• AI tools like CombineHealth's Jessica and Amy help fix this at the source by generating accurate MDM narratives, flagging gaps, and coding with full explainability.
Picture this: it’s a packed Tuesday morning. Providers are double-booked, inboxes are overflowing, and patients are waiting in hallways.
A family medicine physician stabilizes a patient with worsening asthma, personally interprets the peak flow, reviews last year’s pulmonology notes, adjusts meds, and schedules close follow-up. Five minutes later, the note ends up saying: “Asthma follow-up. Stable. Continue meds.”
The visit was High-Complexity MDM. But the documentation reads like Level 2. That gap quietly drains hundreds of thousands in revenue across a system.
Clinicians are doing the cognitive work. The problem is getting that thinking into the chart—consistently, clearly, and in a way payers will actually recognize.
This guide breaks down why medical decision making drives healthcare reimbursement. We'll also showcase the strategies that can turn everyday clinical decisions into the revenue and risk adjustment you’ve already earned.
What Is Medical Decision Making (MDM)?
Medical Decision Making (MDM) measures the cognitive effort it takes to arrive at a diagnosis, interpret data, and assess patient risk. Instead of rewarding longer notes or exhaustive physical exams, the current CPT framework (updated in 2021, 2023, and continuing through 2025) centers payment on the complexity of a provider’s clinical thinking.
A clinician may perform only a brief exam yet still legitimately bill a Level 5 visit if the clinical reasoning is complex. Conversely, a lengthy, detailed physical exam will still fall to Level 2 if the decision-making is straightforward.
Why Is Medical Decision Making Important?
Medical Decision Making (MDM) matters because it determines the E/M level—and, by extension, reimbursement, audit exposure, and the accuracy of clinical documentation. When MDM is under-documented or miscoded, organizations leave significant revenue unrecognized. When it’s overstated, they invite compliance risk, audits, and potential False Claims Act exposure.

MDM also strengthens audit defense. RAC, CERT, and payer reviews zero in on whether the documentation supports the coded level.
Beyond reimbursement, strong MDM contributes to care quality by:
- Structuring clinical decisions around risk
- Guiding timely escalation
- Reinforcing evidence-based practice
For RCM teams, consistent MDM documentation reduces coder ambiguity, improves first-pass yield, and cuts avoidable rework.
Accurate MDM documentation also plays a direct role in strengthening an organization’s Case Mix Index (CMI) and its performance under value-based contracts.
CMI is a risk-adjustment score, and payers use it to decide how much they’ll pay you to manage your population. When clinicians under-document MDM, your organization silently loses HCCs (Hierarchical Condition Categories). And when HCCs drop, CMI drops with them.
The financial implications are enormous. Even a small dip in CMI can mean millions in forfeited value-based revenue. This means weaker Medicare Advantage payments, lower shared-savings payouts, and poorer positioning in managed-care contract negotiations.
How Does Medical Decision Making Work in Practice?
In real clinical encounters, Medical Decision Making (MDM) reflects a clinician's structured narrative of how they reason through:
- what’s happening with a patient
- what could be causing it
- what information is needed
- what to do next
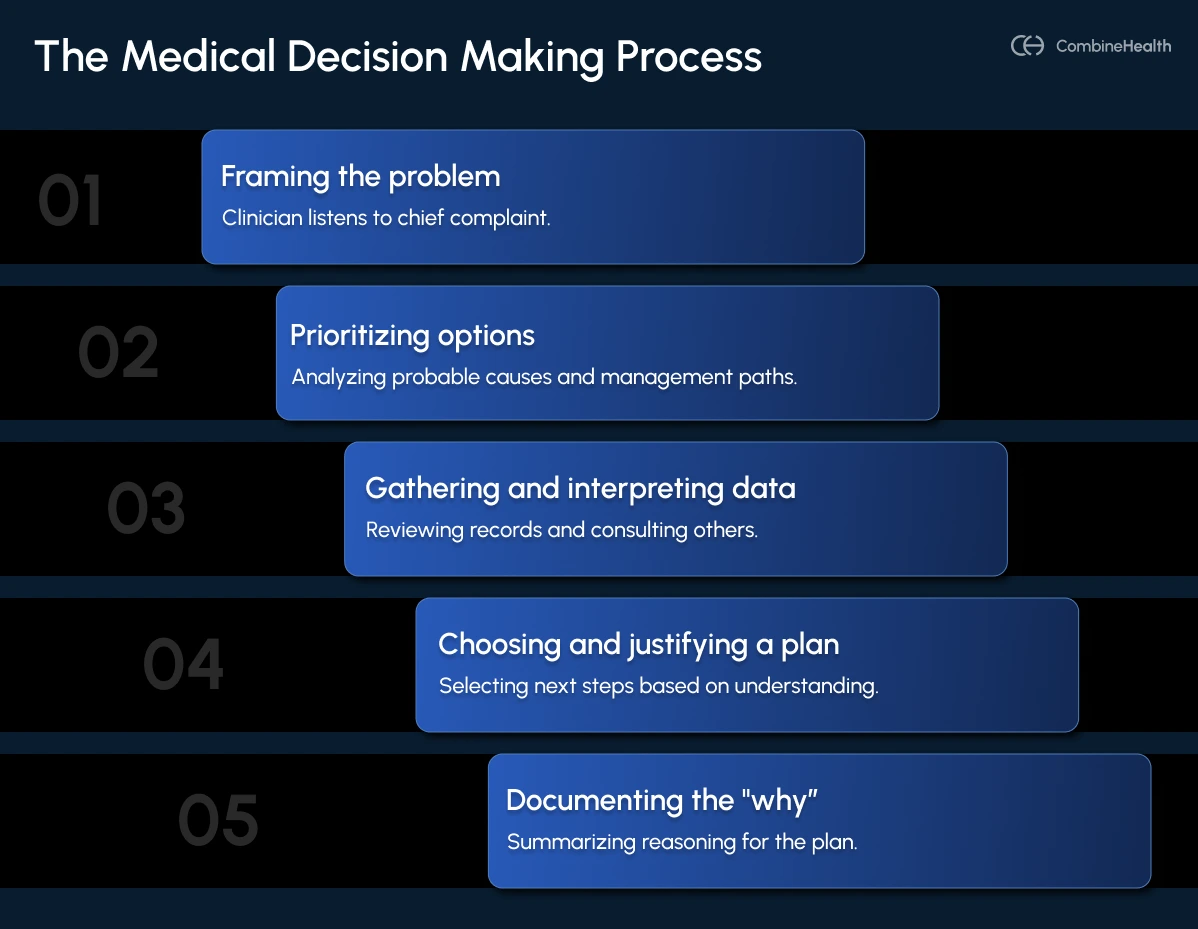
Here's how the medical decision making process typically unfolds:
- Framing the problem: The clinician listens to the chief complaint and short history. Then, they identify one or more working problems (e.g., new chest pain, worsening sugars, or a medication refill with adherence concerns).
- Prioritizing options: The clinician analyzes probable causes and management paths (eg, differential diagnoses, tests, treatments, referrals) and ranks what’s most likely, most urgent, or potentially dangerous.
- Gathering and interpreting data: The clinician reviews prior records, labs, imaging, consult notes, and today’s vitals and exam. They may also need to speak with family members or other clinicians when additional context is needed.
- Choosing and justifying a plan: Based on a refined understanding, the clinician selects the next steps—medication changes, diagnostics, consults, or even hospitalization. They balance benefits, harms, and patient-specific risks.
- Documenting the "why": The assessment/plan summarizes the reasoning: what the clinician believes is happening, why they believe it, and why today’s plan is safe and appropriate.
What Is the "2 out of 3" Rule to Determine Medical Decision Making Levels?
The “2 out of 3” rule is the backbone of MDM level selection. To bill a specific level (such as Moderate or High complexity), the documentation must support any two of the three MDM elements.
This framework gives clinicians flexibility, but it also opens the door to missed opportunities if documentation isn’t precise.
Example:
A visit may involve moderate data (multiple tests, external note review) and moderate risk (prescription drug management). If the problems addressed are documented vaguely as “routine follow-up,” the encounter may default to a lower-coded level—even if the clinical thinking was more complex.
The next section breaks down all three MDM elements and the specific cases when they're applicable.
Key Elements That Define Medical Decision Making
Medical decision making in healthcare is built on three core elements:
Element 1: Number and Complexity of Problems Addressed
This element captures the nature and severity of the conditions the clinician is evaluating or treating during the encounter. The complexity of problems is categorized as showcased in the table below:
Note: The distinction between “stable” and “uncontrolled” is worth millions across a health system. Documentation must clearly state status and severity to avoid revenue loss.
Element 2: Amount and/or Complexity of Data to be Reviewed
This reflects the clinician’s work in gathering, interpreting, and synthesizing information. It includes three categories (showcased in the table below):
Element 3: Risk of Complications or Morbidity/Mortality
This evaluates the inherent risk in the patient’s management plan—not just their condition, but what the clinician decides to do.
Here's how the complications can be categorized:
Time-Based E/M vs. MDM-Based E/M: When To Choose What?
Clinicians now have two compliant paths for selecting an E/M level: time or Medical Decision Making (MDM).

Use time-based E/M when:
- The visit is dominated by counseling, care coordination, or medication discussions.
- The medical complexity is low, but the provider spends significant face-to-face or non–face-to-face time (e.g., discussing a new cancer diagnosis, coordinating home health).
- Documentation of time is clear and easy to capture through the EHR.
Use MDM-based E/M when:
- The complexity of thinking is high—even if the visit is short.
- The clinician is weighing multiple diagnoses, reviewing data, or managing moderate/high-risk decisions (e.g., medication changes, escalation of care).
- Independent interpretation, external discussions, or SDOH factors drive risk.
Common Challenges in MDM Documentation
Five common challenges often undermine the accuracy of MDM documentation and revenue integrity:
1. Cloned or Template-Heavy Notes
Copy-pasted MDM narratives trigger payer NLP tools that flag identical language across claims. When dozens of notes look the same, auditors assume systematic misrepresentation, leading to downgrades, denials, or even FCA exposure.
Solution: Use structured templates with problem-specific prompts (e.g., describe today’s unique problem, tests reviewed, and risk considerations).
2. Vague Data Documentation
Generic lines like “labs reviewed” don’t meet CPT thresholds. Auditors count distinct data elements; if none are explicitly listed, the data score defaults to zero.
Solution: Add a dedicated "Data Reviewed" section listing each test, source, date, and interpretation.
Example:
DATA REVIEWED:
1. [Unique source 1 - date]: Brief findings
2. [Unique test 1 - date]: Result and interpretation
3. [External discussion]: Provider name and key point
3. Missing SDOH Documentation
Social Determinants of Health (SDOH) factors can legitimately raise risk from Low to Moderate or High—but only when the note explicitly links them to management complexity.
Solution: Incorporate an SDOH checklist plus a brief statement on how those barriers affect today’s care plan.
Example:
SOCIAL DETERMINANTS ASSESSMENT:
Housing: Stable / Unstable / Homeless
Food Security: Secure / Insecure / Food Insecure
Transportation: Adequate / Limited / None
Language: English / [Other] / Interpreter Needed
Substance Use: None / Active / In Recovery
IMPACT ON TODAY'S MANAGEMENT:
[Specific description of how SDOH affects treatment options or risk]
4. Undocumented Independent Interpretation
Providers often interpret EKGs or labs but document only “results reviewed,” forfeiting Category 2 data credit.
Solution: Add a simple Independent Interpretation line describing the clinician’s findings.
Example:
- EKG interpreted by me: Normal sinus rhythm, LAFB, no acute ischemic changes
- Troponin result (0.01) interpreted in context of clinical presentation: negative for acute MI
5. High-Level Coding Without Risk Justification
Coding Level 4/5 without documenting the risk drivers triggers audits and extrapolated recoupments.
Solution: Review high-level codes against a Medical Necessity Checklist covering problems, data, risk factors, and clinical work performed.
Example:
LEVEL 4/5 MEDICAL NECESSITY CHECKLIST:
Problem(s) addressed meet "Moderate/High" threshold (exacerbation, acute/systemic, or multiple comorbidities)
Data documented includes ≥2 of 3 categories (tests, independent interpretation, external discussion)
Risk element explicitly described (prescription drug monitoring, surgery decision, hospitalization, SDOH impact)
Note reflects substantive clinical work consistent with time spent (if time-based billing)
CombineHealth’s AI Medical Coding Agent Amy provides line-by-line rationale and evidence behind each of her coding decisions.
How AI Can Help in MDM Documentation and Coding
Thoughtfully designed solutions can take a lot of the busywork out of documentation and coding, helping clinicians focus on care while strengthening revenue integrity. Here are three practical ways AI can make a difference:
1. Ambient Listening and Automated Note Generation
AI tools can transcribe the physician–patient conversation in real time and automatically draft the MDM narrative.
Here's how it typically works:
- The conversation is transcribed during the encounter.
- Key details like problems, data reviewed, independent interpretations, and risk factors are pulled into a draft MDM summary.
- The clinician reviews and finalizes the note.
Jessica, CombineHealth’s AI scribing agent, listens to provider–patient conversations in the background and converts them into structured, EHR-ready notes.
2. Coding Assistance with Human Review
Automated coding tools read the clinical note, identify key elements, and suggest an E/M level or diagnosis list for a coder to validate.
Amy, CombineHealth’s AI medical coding agent, reads encounter notes directly from the EHR and recommends precise MDM levels and codes across all outpatient coding systems.
3. Compliance Pattern Detection
These systems monitor billing patterns and flag potential issues before claims go out the door. This way, the risky coding trends are caught early, and overpayments and recoupments can be avoided.
Build a Stronger MDM Workflow Using AI
MDM now decides whether your organization captures the value of the care it delivers—or leaves it on the table. Fix that, and everything improves: fewer denials, higher E/M capture, better CMI, and cleaner audits.
Ready to tighten documentation, eliminate MDM guesswork, and lift revenue without adding staff?
Book a demo with CombineHealth and see how our AI agents can transform your documentation and coding workflow in weeks!
FAQs
Describe a typical workflow for clinical decision-making at the point of care?
Clinician identifies the problem, reviews history/exam and prior data, uses point-of-care tools or guidelines as needed, weighs options and risks with the patient, then selects and documents a plan in the EHR in real time.
How to document MDM to support higher E/M levels?
Clearly state each problem’s status, list key data reviewed/ordered (tests, notes, discussions), and explicitly describe risk/management rationale (e.g., med changes, monitoring, escalation decisions), so the medical necessity for a higher level is obvious and traceable.
How does clinical decision support integrate with MDM documentation?
CDS surfaces guideline-based suggestions, risk scores, and order sets inside the EHR; accepted recommendations and rationale flow into the note, helping structure MDM text and ensuring documentation aligns with evidence-based decisions and payer expectations.
Common MDM documentation errors that trigger audits?
Frequent issues include overcoding without clear risk justification, vague or templated MDM text, missing linkage between problems and data reviewed, and incomplete documentation of medical necessity for high-level visits, all of which raise payer audit flags.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










