The Complete Guide to E&M Coding in 2025
Learn the basics of E/M coding, the 2025 updates, documentation rules, and payer audit tips to improve accuracy, prevent denials, and protect healthcare revenue.
November 3, 2025


Key Takeaways:
• E/M codes convert clinical complexity into billable CPT values; choose levels using MDM or total time per 2025 rules.
• Accurate documentation (reason for visit, MDM or time statement, assessment/plan, signature) is the top defense against denials.
• New 2025 telehealth codes (98000–98015) replaced old telephone codes; document mode, consent, and duration.
• Common denials stem from missing MDM detail, vague time notes, modifier misuse (25/59), and ICD-10 nonspecificity.
• Payers use automated downcoding and targeted audits (Cigna, Aetna, CERT); proactive audits and benchmarking reduce risk.
Medical billing errors are rarely about effort, but more about complexity. And E&M coding is the most frequently used and most scrutinized category in medical billing.
Every visit, note, and decision a provider documents has a financial translation, and when even one detail is missed, the ripple effects can be costly. Now, layer in 2025’s new CPT codes, telehealth expansions, and payer-specific downcoding policies, the margin for error gets even smaller.
But don’t worry, there are practical ways to select the right E&M code, stay compliant, and protect your healthcare organization’s revenue.
This guide breaks down every major component of E/M coding in 2025—from documentation requirements and code selection to payer audits and denial prevention—in the exact order we recommend tackling them.
Let's get into them all one by one.
What Is E&M Coding?
E&M coding is how healthcare providers get paid for non-procedural visits, such as office visits, hospital admissions, and telemedicine consultations.
These E/M codes are maintained by the American Medical Association (AMA) under the Current Procedural Terminology (CPT) system and are used for billing for patient encounters that involve evaluating a patient’s health condition and managing their care.
.webp)
E/M codes translate the clinical complexity of a patient encounter into a numeric value that represents provider work, resource utilization, and risk. Each code level reflects the extent of medical decision-making (MDM) or time spent on the date of service.
Why Does E/M Coding Matter?
E/M coding is one of the most frequently used and most complex areas of medical coding, since it’s based on the provider’s documentation rather than a single, straightforward procedure.
Accurate E&M coding directly impacts:
- Reimbursement Accuracy: Each E&M code has a defined relative value unit (RVU) and corresponding payment rate. Selecting the correct level ensures providers are compensated appropriately for the work performed.
- Compliance and Audit Readiness: E&M is one of the most audited billing categories by the CMS and private payers.
- Revenue Integrity: Undercoding results in lost revenue, while overcoding can trigger denials, recoupments, or penalties.
- Operational Efficiency: E&M accuracy reduces claim rework, accelerates payments, and maintains clean claim rates above industry benchmarks.
Evaluation and Management Coding Examples
Evaluation and management codes are typically divided by setting and patient type:
Below are real-world examples showing how E&M levels differ across encounters, specialties, and documentation depth:
Case 1: Primary Care
A patient with controlled hypertension visits for medication refills and blood pressure monitoring. No new symptoms are reported, and no additional tests are ordered.
E&M Code: 99213 (Established patient, low MDM)
Case 2: Primary Care With Complexity
A 72-year-old patient presents for follow-up of type 2 diabetes, hypertension, and chronic kidney disease (CKD Stage 3). The provider reviews recent labs, adjusts insulin dosage, and coordinates with a nephrologist.
E&M Code: 99215 (Established patient, high MDM)
Case 3: Behavioral Health (Telehealth Visit)
A psychiatrist conducts a 20-minute audio-video telemedicine session with a patient being treated for major depressive disorder. Medication adherence and side effects are reviewed; no acute safety concerns.
E&M Code: 98005 (Established patient, telehealth, low MDM)
Case 4: Emergency Department (In-Person Evaluation)
A patient arrives with shortness of breath and chest pain. The ED physician orders an ECG, chest X-ray, and labs, interprets the results, and initiates a cardiology consult for possible acute coronary syndrome.
E&M Code: 99285 (Emergency Department, high MDM)
Recommended Reading: Evolution of RCM in the emergency department and where AI can help
Case 5: Surgery Clinic (Pre-Operative Consultation)
A general surgeon evaluates a patient for an elective laparoscopic cholecystectomy. The visit involves reviewing prior imaging, explaining surgical risks, and obtaining informed consent.
E&M Code: 99204 (New patient, moderate MDM)
What Are The Components Involved in the E/M Code Selection?
Starting in 2021 and reaffirmed by the 2025 AMA CPT guidelines, providers can select Evaluation and Management (E&M) levels using either total time spent on the date of service or Medical Decision Making (MDM) complexity—whichever most accurately represents the encounter.
Here’s what they each mean and when they’re used:
1. Medical Decision Making (MDM)
MDM represents the complexity of establishing a diagnosis, evaluating data, and determining management options. It is the most commonly used method for E&M selection and is based on three elements:
- Number and severity of conditions evaluated
- Records, tests, or external physician discussions considered in decision-making
- Risk involved, like potential for morbidity, mortality, or treatment complications
To determine the E/M code, at least two of the three MDM elements must meet or exceed the requirements for a specific level of service.
Below is a breakdown of how the severity of conditions and their MDM levels are evaluated:
2. Time-Based Evaluation
When a provider’s effort is primarily driven by counseling, care coordination, or documentation time rather than MDM complexity, time-based coding is appropriate. Time refers to the total time personally spent by the provider on the date of service, including both face-to-face and non-face-to-face work.
Countable activities include:
- Reviewing prior notes and test results
- Performing the patient exam
- Counseling and educating the patient or family
- Documenting in the EHR
- Communicating with other healthcare professionals
- Ordering tests, medications, or referrals
Time-Based E&M vs. MDM-Based E&M: When To Choose What?
Both time-based E&M and MDM-based E&M selection are valid ways to code for the services provided, but they serve different purposes.

Here’s how both approaches compare with one another and when to choose what:
The choice between Time and MDM based E and M coding depends on what drives the encounter’s complexity and resource use.
Example:
For prolonged patient counseling that involves lifestyle changes, chronic disease education, a time-based evaluation would be a better choice. That’s because in this case, the clinical reasoning is less complex but time-intensive.
However, for multiple comorbidities requiring diagnostic analysis and data review, an MDM-based code selection would be appropriate.
How To Select the Correct E&M Code?
The key to selecting the right E/M code is aligning clinical documentation with the official code descriptors, ensuring the record clearly supports the code billed.
Here’s what the process typically looks like:
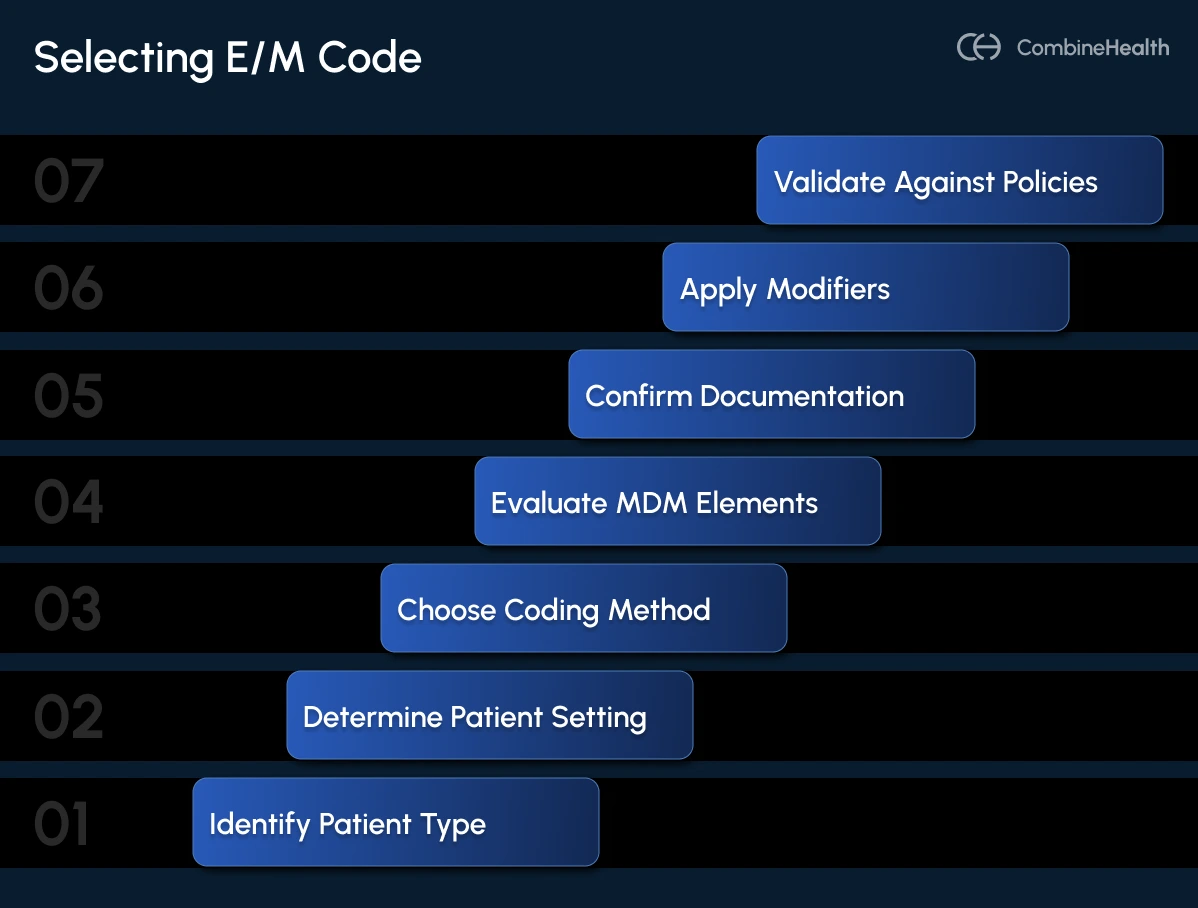
- Identify Patient Type: Determine whether the patient is new or established.
- Determine the Setting: Confirm if the encounter is office-based, inpatient, telehealth, or emergency.
- Choose the Coding Method: Decide whether MDM or time better reflects the service rendered.
- Evaluate the MDM Complexity: Assess the number and complexity of problems, data, and risk. You must meet or exceed two of the three elements to support a given level.
- Verify Time Thresholds: If using time-based selection, use total provider time spent on the date of service—including chart review, counseling, and documentation.
- Confirm Documentation Support: Verify that the record supports the chosen level of complexity or total time.
- Apply Modifiers (if applicable): Use Modifier 25 for separately identifiable E&M on the same day as a procedure. Also, use G2211 as an add-on code for visit complexity related to longitudinal patient care.
- Validate Against Payer Policies: Some payers, such as Cigna and Aetna, apply automated downcoding algorithms that require explicit documentation of MDM elements.
Check out this E/M Calculator by AAPC that helps you determine the final E/M code by inputting encounter details.
What Are the E&M Documentation Requirements?
Every E&M record must be complete, specific, and internally consistent.
The CMS defines proper documentation through a set of foundational principles that apply to all E&M services:
- Ensure legibility and completeness of every record.
- Clearly state the reason for the visit, assessment, and plan.
- Record risk factors, treatment changes, and patient response.
- Match diagnosis and procedure codes precisely to the documented findings.
Documentation Based on MDM
When coding is based on MDM, the documentation must explicitly support the three MDM elements defined by the AMA:
1. Problems Addressed
- Clearly identify each condition evaluated during the encounter
- Indicate whether it is new, chronic, stable, worsening, or self-limited
- Include supporting data, such as severity or duration
Example: “Chronic kidney disease — Stage 3, worsening with elevated creatinine”
2. Data Reviewed and Analyzed
- List each test, imaging study, or consultation reviewed
- Specify if the data were independently interpreted or discussed with external clinicians
Example: “Reviewed recent nephrology note and lab panel from 10/15/25; discussed management changes with Dr. Ryan.”
3. Risk of Complications and Morbidity
Describe treatment options considered, changes in therapy, and potential complications.
Example: “Initiated insulin; discussed risk of hypoglycemia.”
Documentation Based on Time
When using time-based coding, the provider must document total time spent on the date of service and detail qualifying activities.
Example: “I personally spent 42 minutes on the calendar day of the encounter, including 15 minutes reviewing prior labs, 10 minutes patient counseling, and 17 minutes documentation.”
Do not include:
- Staff-only time
- Time spent on separately billable procedures
- Non-clinical administrative work
MIPS compliance and E&M documentation
Accurate E&M documentation directly impacts Merit-based Incentive Payment System (MIPS) performance scores. Each encounter must demonstrate:
- Quality
- Cost-efficiency
- Clinical reasoning
All these factors help satisfy MIPS quality measures, particularly those tied to chronic disease management, preventive services, and care coordination.
Precise E&M documentation not only drives reimbursement accuracy but also protects incentive payments and future participation eligibility under evolving MIPS Value Pathways (MVP) frameworks.
What Are the Fundamental Changes to E&M Coding Guidelines in 2025?
The 2025 CPT and CMS updates represent one of the most significant expansions of Evaluation & Management (E&M) services since the 2021 transition to MDM-based coding.
These changes reflect a broader shift toward virtual-care inclusion, longitudinal patient management, and outcome-driven documentation.
Introduction of New Telemedicine Evaluation and Management Codes
The 2025 CPT code set introduces a dedicated family of telemedicine evaluation and management codes to differentiate between audio-video and audio-only visits.
Deletion of Outdated Telephone Assessment E/M Codes
CPT codes 99441–99443 (telephone evaluation and management) are deleted as of January 1, 2025. These have been replaced by 98008–98015 to align with the growing hybrid-care model and ensure time-based parity with in-person visits.
Revised Documentation Expectations
The 2025 AMA update continues the 2021 shift toward clinically relevant documentation over volume.
How Do Modifiers Impact E&M Billing and Reimbursement?
Modifiers provide essential context to an Evaluation & Management (E&M) service, signaling to payers that a visit included distinct or additional work beyond the standard encounter. When applied correctly, modifiers ensure providers are reimbursed appropriately.
Here are the common modifiers used in E/M billing:
1. Modifier 25: Separately Identifiable E&M Service
The use of Modifer 25 indicates that the E&M service was above and beyond the usual preoperative or postoperative evaluation associated with a procedure performed on the same day.
Some appropriate use cases:
- When an E&M visit addresses a new or unrelated problem on the same day as a minor procedure.
- When the documentation clearly distinguishes the E&M assessment from the procedure itself.
- When both services are medically necessary and properly documented.
Example:
A patient visits for an ear infection and, during the same encounter, receives a mole removal. In this case, the evaluation can be billed with 99213-25, and the mole removal with the procedure code.
2. Modifier 59: Distinct Procedural Service
The use of modifier 59 denotes that a procedure or service is separate and distinct from another procedure performed on the same day, even when both codes normally bundle under National Correct Coding Initiative (NCCI) edits.
The differences between Modifier 25 and 59:
- Modifier 59 applies to procedures, not E&M services.
- For E&M services performed on the same day as a procedure, Modifier 25 should be used instead.
Example:
If a provider performs two procedures on the same day that would normally be bundled, Modifier 59 may be appended to the secondary code to justify payment.
3. G2211: Visit Complexity Add-On Code
G2211 is not technically a modifier, but it acts as an add-on code for visit complexity. It reflects the additional work associated with longitudinal or ongoing patient management during office or outpatient visits.
When you can bill G2211:
- When the provider manages ongoing, complex, or chronic conditions over multiple visits.
- When acting as the patient’s continuing focal point of care.
- When the service is separate from acute or procedural-only care.
Why E/M Coding Is So Challenging?
Even with the AMA’s simplification of documentation rules and the 2021 shift to Medical Decision Making (MDM)-based coding, E/M coding issues are one of the top causes of claim denials and compliance audits.
Common challenges include:
- Inconsistent or incomplete documentation from providers that often lacks details like reason for encounter, relevant history, exam findings, and plan of care
- Frequent changes in payer-specific E/M rules between 2021 and 2025
- “Gray areas” in medical necessity justification, as each of the three MDM elements depends on detailed provider documentation
- Deciding between coding by time or MDM by determining when counseling or coordination outweighs diagnostic complexity
- Lack of time for coders to review complex notes manually
- Provider-led self-coding errors (especially in FQHCs and outpatient settings)
- Automated payer downcoding that automatically reduces high-level E&M claims when documentation doesn’t precisely meet AMA or CMS criteria
- Payers increasingly deploying AI-based claim audits to detect inconsistencies between documentation and billed codes
Common Denials in E&M Billing
Below are some common denials happening in E/M billing:
1. Documentation Errors
Documentation gaps in E/M billing prevent coders and payers from validating the billed level of service.
Some common documentation-related issues include:
- Missing chief complaint or HPI
- Incomplete MDM details
- Vague time statements
- Illegible or unsigned documentation
- Copy-paste notes
CombineHealth’s AI Medical Coding Agent Amy automatically reviews encounter notes for missing MDM, time, or modifier elements and suggests code-level adjustments based on payer-specific logic.
2. Medical Necessity Denials
Medical necessity is the “overarching criterion” for payment for E/M services. Some common examples of unjustified medical necessity include:
- Level 4 or 5 billed for minor or stable conditions
- High-complexity E and M codes used without corresponding MDM or risk documentation
- Diagnosis code (ICD-10) lacks specificity or fails to support service level
CombineHealth’s AI Appeals Agent Rachel extracts subtle references from provider notes to generate medical necessity reasoning.
3. Modifier-Related Denials
Modifiers 25 and 59 are among the most common sources of E&M denials due to misuse or omission.
For example, a provider bills 99214 with a minor procedure but fails to document a separate assessment, and as a result, the payer bundles the E&M and denies the claim.
CombineHealth’s AI Medical Billing Agent Mark applies payor-specific billing SOPs, validates codes & modifiers, and prepares charges for claim submission.
4. Incorrect Level of Service
Both upcoding (billing higher than documentation supports) and undercoding (billing lower than complexity) are costly. As a result, payer downcoding algorithms automatically lower levels if MDM documentation is vague or missing.
CombineHealth’s AI Medical Coding Agent Amy provides line-by-line rationale and evidence behind each of her coding decisions.
E&M Audit Programs by Different Payers
Payer audit programs have become more automated, frequent, and stringent. Here are some examples:
1. Cigna’s E&M Coding Accuracy Policy
Effective October 1, 2025, Cigna’s automated downcoding policy (R49) evaluates high-level E&M claims (99204, 99205, 99214, 99215) using AI algorithms that scan claim data for compliance with AMA 2025 guidelines.
Key features of the program:
- Automatically downcodes unsupported E&M claims by one level.
- Does not require clinical record review before reduction.
- Providers may appeal by submitting medical records for reconsideration.
2. Aetna Claim and Code Review Program
Launched concurrently with Cigna’s policy, Aetna’s program targets Level 4 and 5 E&M visits across multiple specialties.
Audit focus areas include:
- Consistency between MDM documentation and billed level
- Completeness of assessment and plan sections
- Overuse of high-level visits relative to specialty norms
3. Medicare CERT (Comprehensive Error Rate Testing)
CMS’s CERT program audits a random sample of Medicare claims annually to measure improper payment rates. E and M codes like 99214 consistently rank among the top error categories.
E/M Coding Compliance and Audit Best Practices
Follow these best practices to strengthen your E/M coding and billing workflows:
1. Implement Internal E&M Audits Regularly
Focus on verifying MDM accuracy, time-based documentation, and modifier use. Once done, compile these findings into a structured report shared with compliance, coding, and clinical leadership.
Over time, these audits reveal provider-specific trends—such as habitual undercoding or inconsistent MDM descriptions—that can be corrected through focused education before external audits occur.
2. Use AI-Powered E and M Code Validation Tools
Use AI-assisted RCM Platforms to analyze encounter notes in real time, verify MDM completeness, and detect inconsistencies between documented risk, time, and diagnosis codes. The goal is to reduce manual errors by flagging missing chief complaints, vague MDM narratives, or unsupported time entries before claim submission.
For healthcare organizations handling large volumes of claims on a daily/weekly basis, these tools can help ensure payer-specific policy alignment by automatically applying the correct modifiers and identifying conflicts.
3. Educate Providers Continuously
Continuous provider education is critical to maintaining compliant E&M coding—especially amid yearly CPT and CMS updates. Make sure each provider undergoes refresher training at least twice a year, covering new documentation rules, payer audit trends, and real case examples from internal audits.
4. Benchmark Code Distributions
Benchmarking E&M utilization is one of the most effective ways to identify compliance risks early. Each specialty has an expected “bell curve” of E&M code usage—for instance, family medicine typically bills 99213–99214 most frequently, while emergency departments skew toward 99284–99285.
5. Track E/M Denial Trends
Establish an E&M denial analytics dashboard that categorizes issues by type (medical necessity, modifier, documentation, or coding level) and calculates both denial frequency and financial impact. Pair quantitative data with qualitative root-cause analysis from appeal outcomes to understand why certain payers or providers generate more denials.
For example, if a pattern emerges where 99214 claims are frequently rejected for “insufficient MDM,” it signals a documentation training need rather than a billing issue.
.webp)
Ready To Strengthen Your E&M Coding Compliance?
E&M documentation shouldn’t be a guessing game—and it doesn’t have to drain your team’s time or revenue. That’s why CombineHealth’s AI Agents help streamline your E/M coding and billing accuracy.
From Amy, the AI Medical Coder who ensures compliant, payer-specific code selection, to Mark, the AI Biller who validates claims and manages denials—our AI Workforce works together to reduce errors, accelerate reimbursements, and protect revenue integrity across every encounter.
Book a demo today!
FAQs
What is the difference between a CPT code and an E/M code?
CPT codes describe all medical services and procedures, while E and M codes are a specific subset of CPT codes used to report patient evaluation and management visits based on complexity, time, and medical decision-making.
What is medical decision-making in E&M coding?
Medical decision-making (MDM) reflects the complexity of diagnosing and managing a patient’s condition. It considers three elements: problems addressed, data reviewed, and risk of complications or morbidity.
What are the new E&M guidelines for 2025?
The 2025 CPT update introduces new telehealth codes (98000–98015), deletes telephone visit codes (99441–99443), expands G2211 usage, and clarifies “medically appropriate” history and exam documentation.
What are some common denial reasons related to E&M coding?
Frequent denial causes include missing chief complaints, incomplete MDM, incorrect time documentation, misuse of modifiers (especially 25), vague medical necessity justification, and mismatched ICD-10 specificity.
What is E/M in medical coding?
E/M stands for Evaluation and Management. It refers to a category of CPT codes used to document and bill for non-procedural patient encounters—such as office visits, hospital admissions, and telehealth consultations—based on the complexity of medical decision-making or total time spent providing care.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)









