One Big Beautiful Bill Act: 6 Key Takeaways for FQHCs
Understand the OBBBA’s impact on FQHCs—Medicaid cuts, work requirements, and coverage loss. Adapt by strengthening outreach, improving billing systems, partnering locally, and embracing tech to reduce admin and financial strain.
August 2, 2025


Key Takeaways:
• Massive Medicaid cuts could leave millions of FQHC patients uninsured.
• New work requirements will increase coverage churn and admin burden.
• FQHCs may face service cuts and workforce shortages.
• Rural Health Transformation funds offer limited relief.
• AI tools can help manage eligibility, denials, and documentation workloads.
The "One Big Beautiful Bill Act" (OBBBA), also known as H.R. 1, is a budget reconciliation law signed by President Donald Trump on July 4, 2025. It’s framed as an effort to fix the federal budget.
But while it touches a little bit of everything (taxes, immigration, energy, defense), the biggest shakeups are in healthcare.
And if you’re part of a community health center or an FQHC, the changes headed your way aren’t just policy tweaks. They’re the kind that could completely reshape how you serve patients, staff your clinics, and stay financially afloat.
Here’s an overview of what changes await healthcare workers:
How the Healthcare Sector Is Responding to the OBBBA
According to the bill's backers, Medicaid should primarily serve:
- Children
- People with disabilities
- The elderly
The supporters also highlight some potential benefits of the OBBBA, such as:
- Reduction in federal spending, which might help curb the growing deficit
- Encouraging work and personal responsibility among able-bodied adults
- Reduction in enrollment fraud and misuse of Medicaid benefits
- Streamlining the subsidy system
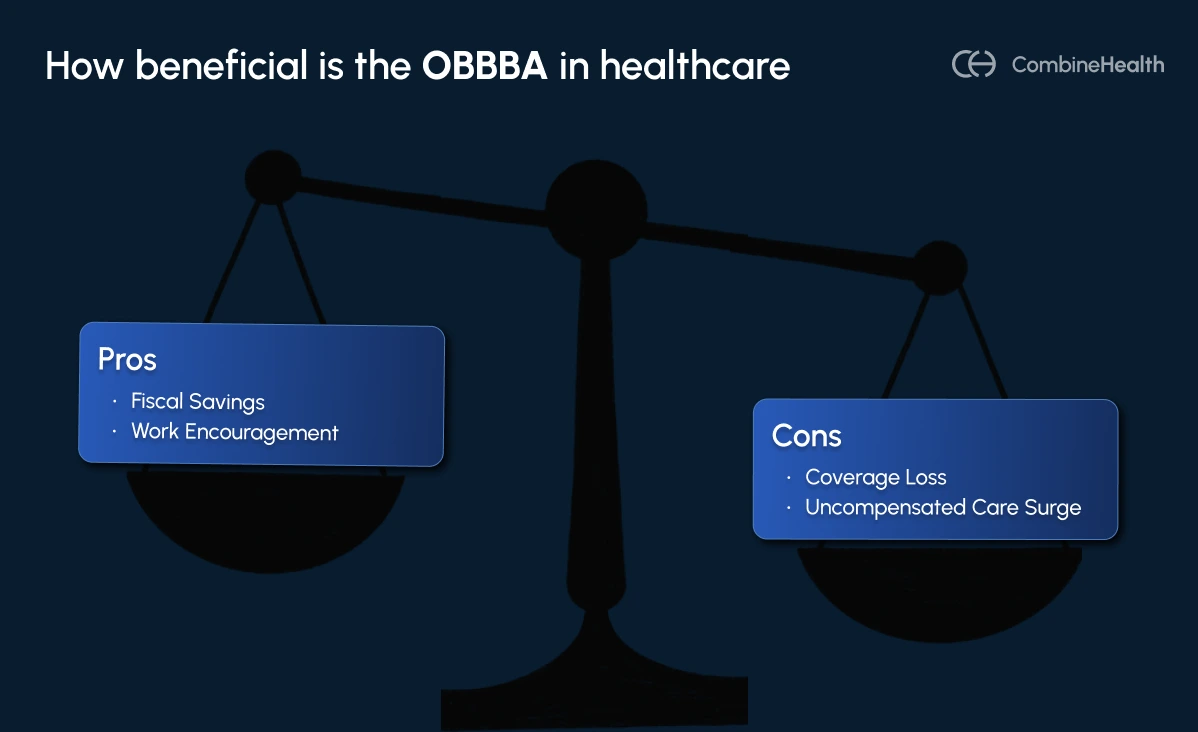
But critics see it differently.
They argue that the new work requirements and paperwork burdens aren’t really about promoting employment—they’re about disqualifying eligible people from coverage[2].
And the data backs this up: most non-elderly Medicaid recipients are already working or in school. Only about 8% fall outside work, school, or caregiving roles[3].
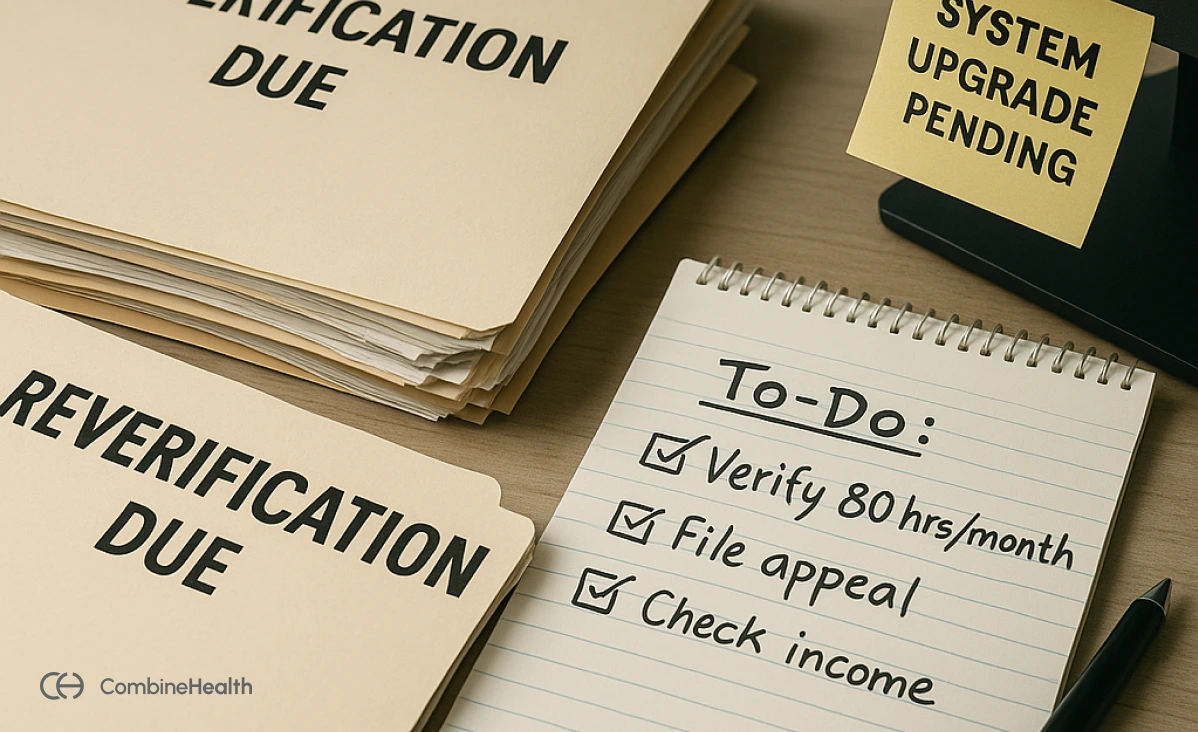
Also, the administrative burden is massive. State Medicaid agencies will need to:
- Upgrade IT systems for tracking work hours and verifying eligibility: Many state officials have raised concerns about their ability to reliably monitor Medicaid enrollees’ work activities, especially given that most existing systems were never built to track complex, real-time employment data at scale[4].
- Handle a surge in procedural dis-enrollments and re-enrollments: As of mid-2024, about 69% of Medicaid coverage losses occurred for procedural reasons, not because people no longer qualified[5].
The American Medical Association (AMA) also warned that the law may turn manageable conditions into life-threatening ones by delaying access to care, calling OBBBA a step in the wrong direction for public health[6].
How The Bill Can Impact FQHCs
As safety net providers for millions of low-income Americans, FQHCs have their operations deeply tied to Medicaid and other federal programs. This makes them especially vulnerable to the bill’s sweeping changes. Here’s how:
1. Medicaid Cuts and Rising Uninsured Populations
The $1 trillion cut to federal Medicaid funding is projected to result in 17 million more uninsured Americans by 2034. In fact, FQHCs nationwide anticipate up to 5.6 million of their patients losing Medicaid due to work requirements[7].
With fewer patients covered, FQHCs will face rising uncompensated care costs. And this puts pressure on already lean budgets that depend heavily on Medicaid reimbursements.
2. Increased Administrative Burden and Coverage Churn
Starting in 2027, the bill introduces work requirements for Medicaid eligibility:
- Non-disabled adults aged 19–55 must complete at least 80 hours per month of work, job training, or community service.
- Eligibility must also be reverified every six months (instead of annually), with stricter checks on address and income.
These new Medicaid rules will likely cause a lot of “procedural churn”. This means people who should qualify for coverage may end up losing it just because they missed some paperwork.
This would be particularly challenging for patients who move often, don’t have a permanent address, or struggle with reading official letters in English. Others may have a job but can’t easily prove they're working the required 80 hours a month.
And when that happens, guess who they turn to? FQHCs.
Health centers will be the ones helping these patients reapply, verify documents, and figure out what went wrong, all while trying to keep the clinic running smoothly.
3. Financial Strain and Risk of Closures
FQHCs already operate on tight margins. And with the expected spike in uninsured patients, these health centers could face serious financial trouble. That might mean tough choices like cutting staff, scaling back services, or, in some cases, shutting down altogether.
The bill does include $50 billion over five years to support rural hospitals and providers like FQHCs through a Rural Health Transformation Program[8]. But compared to the size of the Medicaid cuts, that funding is nowhere near enough.
4. Service-Specific Restrictions
The bill also places limits on what Medicaid will actually cover.
For example, it temporarily bans Medicaid from reimbursing services provided by Planned Parenthood, and it blocks federal Medicaid funds from being used for gender-affirming care.
Many women and LGBTQ+ patients rely on FQHCs for exactly these kinds of services. If those services are suddenly no longer covered, patients may avoid care altogether or be forced to travel farther (or pay out of pocket).
5. Workforce Impact
Many FQHCs may have to rethink staffing, pause hiring, or even let some positions go just to stay financially stable.
And it’s not just about current staff. The bill also puts limits on federal student loans, which could make it harder for future healthcare professionals to enter the field.
That’s a serious concern for FQHCs, many of which already struggle with recruiting and keeping qualified staff. If the pipeline shrinks, the workforce shortage could get even worse.
6. Increased State Financial Responsibility
The OBBBA doesn’t just cut federal spending. It also pushes more responsibility onto individual states to manage and fund programs like Medicaid and SNAP. That means states will have to find ways to cover those costs on their own.
For FQHCs, that creates a ripple effect. If states start pulling funds from public health or tech infrastructure, it could make it harder for health centers to modernize their systems, share data effectively, or even keep up with patient needs.
How FQCHs Can Prepare and Adapt
While the challenges are real, so are the opportunities for forward-looking health centers. Here are a few ways you can navigate the storm while continuing to deliver high-quality care:
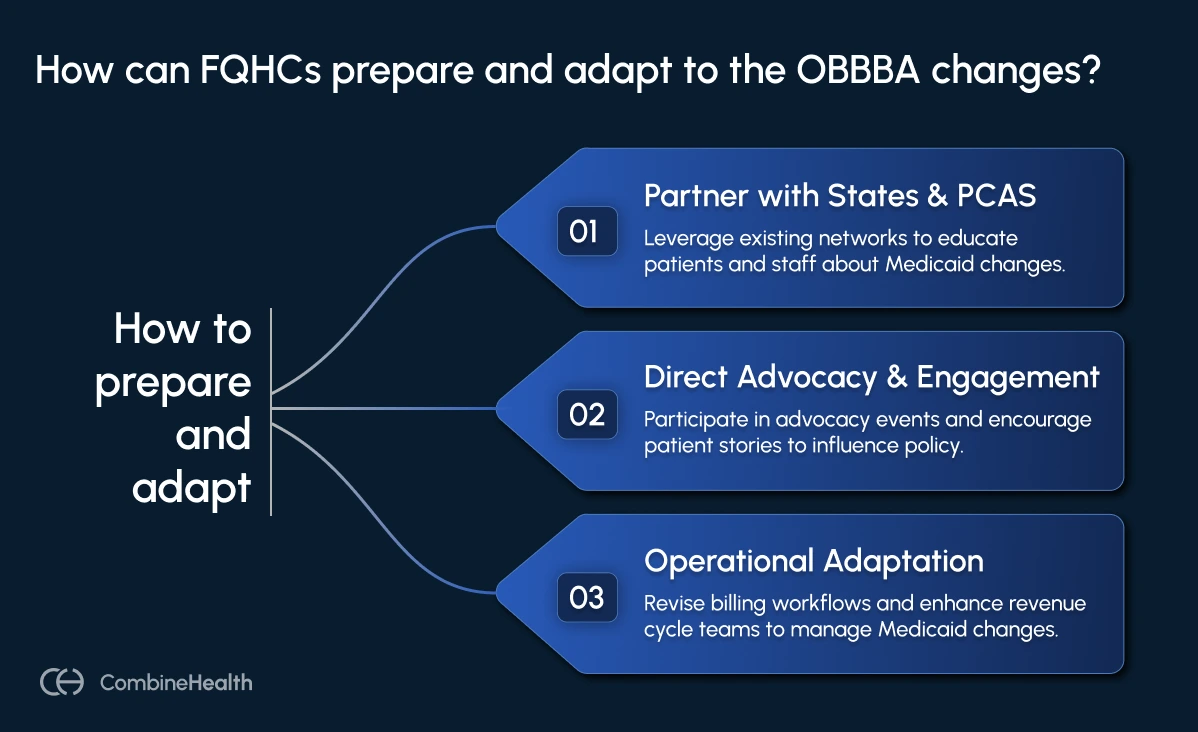
Partner directly with states and Primary Care Associations (PCAs)
As NACHC puts it, one of the smartest moves FQHCs can make right now is to partner with state governments and PCAs to educate patients (and even staff) about the new Medicaid work requirements[9].
The silver lining is that you’re not starting from scratch. Most FQHCs already have an incredible network of outreach and enrollment staff (patient navigators and community health workers) who know exactly how to walk patients through Medicaid renewals. Now’s the time to lean on that expertise and scale it up.
There’s also an opportunity to build bridges with local job training and education programs. By connecting patients to these services, FQHCs can help them meet the 80-hour monthly requirement for Medicaid eligibility.
Direct Advocacy and Community Engagement
Another solid way for FQHCs to step up? Become an Advocacy Center of Excellence (ACE).
FQHC leaders should also get involved in advocacy events—attending NACHC’s fly-ins and PCA-led state advocacy days to speak directly with legislators and push for protections and support.
And it’s not just about the staff; patients’ voices matter too. Encourage patients to share their stories with lawmakers. Real experiences from the communities FQHCs serve are powerful tools for protecting funding and access.
Operational and Strategic Adaptation
To weather the ripple effects of OBBBA, FQHCs will need to think ahead, both operationally and financially.
That means frequent Medicaid eligibility checks and the introduction of work requirements mean more denials and rejected claims are likely. FQHCs will need to revisit their billing workflows and bolster their revenue cycle teams to keep up with the documentation standards.
Also, while the $50 billion Rural Health Transformation Program is small in comparison to the Medicaid cuts, it’s not insignificant. Here’s what healthcare attorney Susannah Gopalan has to say about this[10]:
“OBBBA will not erode the basic Medicaid protections for FQHCs and includes a new program that may benefit FQHCs by helping them fund tech upgrades, care coordination efforts, and workforce development in rural communities.”
The Future of Sustainable Care Lies in Smarter Systems
Everything from eligibility to billing is about to get more complicated for FQHCs. And with limited staff and tight budgets, keeping up won’t be easy.
That’s where an AI-powered solution can be an extra set of hands (and eyes) to handle the administrative heavy-lifting for you. This could include tasks like:
- Tracking frequent eligibility changes
- Understanding denials and their root causes
- Spotting billing errors before they cause denials
- Auto-filling documentation so clinicians can focus on care, not clicks
Curious how AI can support your health center? Let’s talk.
References
[1]AHA. https://www.aha.org/news/headline/2025-07-21-cbo-projects-obbba-increase-uninsured-10-million-federal-deficit-34-trillion#:~:text=The%20Congressional%20Budget%20Office%20today,6, sourced July 31, 2025
[2]Washington Post. https://www.washingtonpost.com/politics/2025/07/10/democrats-try-flip-script-red-tape/, sourced July 31, 2025
[3]American Progress. https://www.americanprogress.org/article/the-truth-about-the-one-big-beautiful-bill-acts-cuts-to-medicaid-and-medicare/#:~:text=adults%20who%20are%20just%20choosing,for%20aging%20parents%20or%20children, sourced July 31, 2025
[4]Governing. https://www.governing.com/policy/states-may-have-trouble-tracking-medicaid-patients-work-status, sourced July 31, 2025
[5]JamaNetwork. https://jamanetwork.com/journals/jama-health-forum/fullarticle/2825467, sourced July 31, 2025
[6]AMA. https://www.ama-assn.org/health-care-advocacy/advocacy-update/july-11-2025-advocacy-update-spotlight-budget-reconciliation#:~:text=Flint%2C%20Michigan%2C%20and%20it%20is,%E2%80%9D, sourced July 31, 2025
[7]Common Wealth Fund. https://www.commonwealthfund.org/blog/2025/community-health-center-patients-medicaid-coverage-work-requirements#:~:text=Over%20the%20five%20years%20following,percent%20of%20CHCs%E2%80%99%20operating%20revenue, sourced July 31, 2025
[8]Health Affairs. https://www.healthaffairs.org/do/10.1377/forefront.20250722.757156/, sourced July 31, 2025
[9]NACHC. https://www.nachc.org/state-impacts-of-the-one-big-beautiful-bill, sourced July 31, 2025
[10]Feldesman. https://www.feldesman.com/the-one-big-beautiful-bill-act-is-approved-by-the-senate-devastating-impacts-for-health-coverage-overall-some-silver-linings-for-fqhcs/#:~:text=This%20legislation%20will%20likely%20result,net%20providers, sourced July 31, 2025
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















