Value-Based Care in Healthcare: A Comprehensive Guide
Discover what value-based care in healthcare means, how it compares to fee-for-service, and what it takes to make the transition.
September 4, 2025


Making the switch to value-based care is no simple task. It involves untangling complex data issues, managing financial risks, reshaping workflows, and most importantly, changing the culture from focusing on quantity to prioritizing quality.
In fact, 86% of physicians are still using the fee-for-service payment model due to adaptation challenges.
In this comprehensive guide, we’ll walk through what value-based care really means, what the transition actually looks like, the different value-based reimbursement models that exist today, and explore the challenges of adopting it.
What is Value-Based Care in Healthcare?
Value-based care is a healthcare model that prioritizes patient outcomes and quality over the volume of services provided. This means healthcare providers get paid for keeping people healthy.
The goal is to help patients maintain their highest possible level of wellness rather than waiting until they are sick, which is often more complex and expensive.
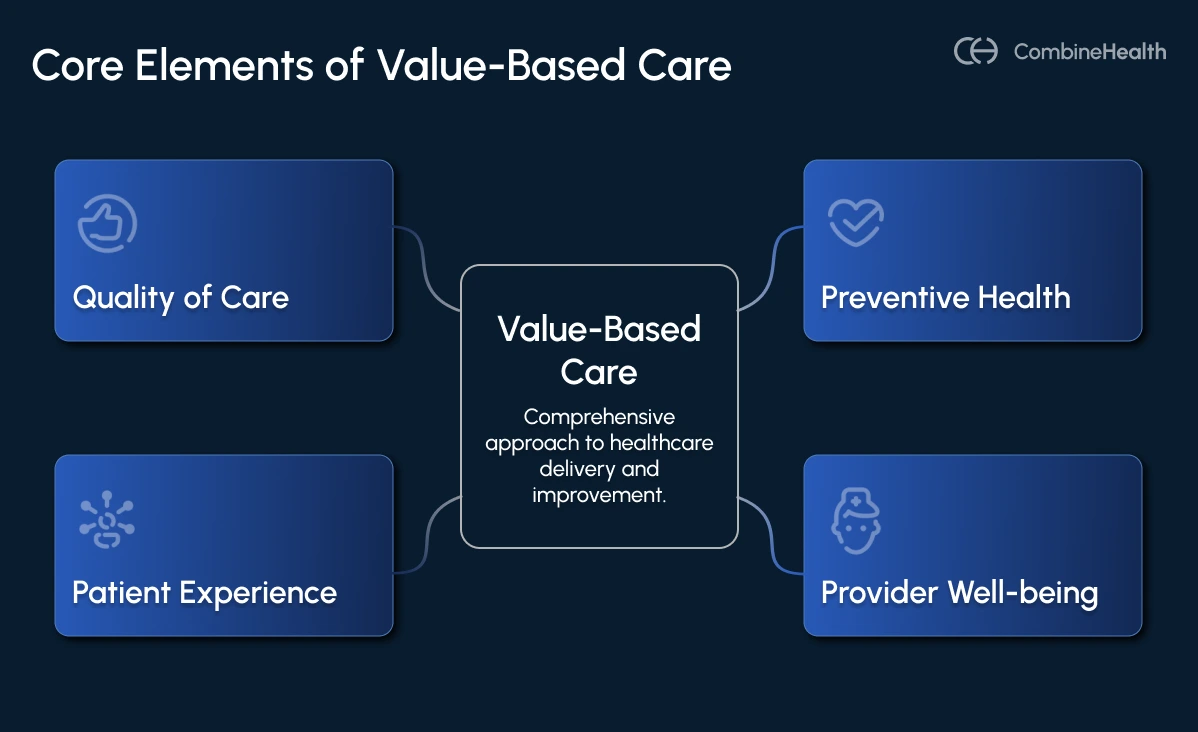
And, it’s not just about achieving these outcomes, but also about how efficiently they’re achieved.
Example:
Two hospitals might both cure a patient, but if one does it with fewer unnecessary tests and better coordination, it’s more “value-based.”
Why is this shift to VBC happening now?
In an AMA Update podcast, Dr Maria Ansari shared that the pandemic really exposed some cracks in the fee-for-service (FFS) model. When people stopped coming in for in-person visits, healthcare organizations saw their revenue take a big hit. Plus, a lot of preventive care got pushed aside as patients delayed regular check-ups and screenings.
Meanwhile, CMS, the biggest player in healthcare payments, is pushing hard for value-based care, aiming to have all patients enrolled in value-based models by 2030.
One big part of that effort is encouraging Medicare beneficiaries to switch to Medicare Advantage, which operates on a value-based platform.
And the results speak for themselves: Medicare Advantage has shown better management of chronic diseases and improved cancer screenings compared to traditional FFS Medicare.
Fee-for-Service vs. Value-Based Care Delivery Model
The shift from fee-for-service to value-based care is transforming revenue cycle management. These two models differ not just in payment methods but in how financial success and patient outcomes are prioritized.
The table below highlights the difference between the two:
How To Make the Transition to Value-Based Care?
The shift from traditional FFS to the VBC model isn’t a flip-the-switch kind of change. The transition is often gradual, deeply complex, and highly dependent on each organization’s infrastructure, leadership, and patient population.
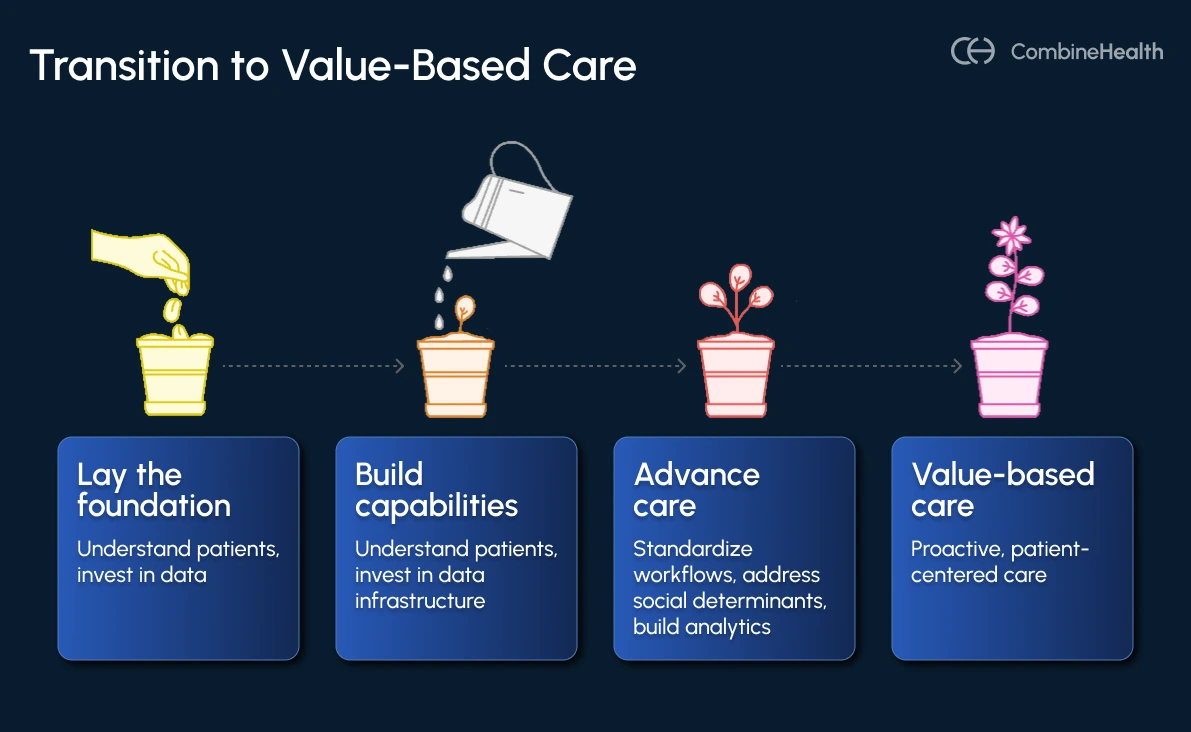
1. Lay the Foundation
Start by really understanding your patient demographics—who they are, how they factor into your payer contracts, and what their health needs look like. Next, invest in a strong data infrastructure that ensures clinical data is timely, accurate, and easily accessible.
Also, cultivate a culture that brings leadership and front-line staff on board with this new approach.
2. Build Capabilities and Optimize Workflows
Move beyond one-size-fits-all care by standardizing clinical workflows around population health.
- Develop population-health-focused care pathways.
- Create analytics and quality teams to identify care gaps, stratify risk, and drive interventions.
- Build relationships with hospitals, specialists, home health providers, and post-acute care facilities
Don’t overlook social determinants of health; screen patients for food insecurity, housing instability, and transportation challenges.
3. Advance to Predictive, Proactive Care
This is where value-based care truly shines. Instead of reacting to illness, leverage predictive analytics and advanced data tools to identify patients at risk before issues escalate.
Use clinical data, social factors, and even remote monitoring to tailor proactive interventions that close care gaps and prevent costly hospitalizations.
Real-World Use Cases of Value-based Care Adoption
Value-based care is more than just a theory; it’s happening right now, transforming health systems across the country. Check the following real-world examples:
Hattiesburg Clinic
Hattiesburg Clinic, a physician-owned group in rural Mississippi, knew the old way of doing healthcare just wasn’t sustainable. They saw rising costs and stagnant outcomes under fee-for-service.
So back in 2007, they started shifting toward value-based care.
But they didn’t dive in headfirst. They took it step by step, starting with Medicare Advantage contracts, then bundled payments, ACOs, and eventually, in 2023, a global budget model.
To make that shift work, they built a strong foundation. They rolled out Epic early on to get better data, created teams focused on care quality and analytics, and used predictive tools to spot high-risk patients before things got serious. They even redesigned care teams, pairing doctors with advanced practice providers to improve coordination, and started screening for social issues like food insecurity or transportation gaps.
And it paid off. Since 2016, they’ve saved Medicare over $66 million, earned $53 million in value-based payments, reduced hospitalizations by 12%, cut readmissions by 30%, improved hypertension control from 54% to 70%, and boosted physician satisfaction above national averages
Geisinger Health System
Geisinger, serving predominantly rural communities across Pennsylvania, knows firsthand how hard it is for patients to access care, with many living in medically underserved areas and facing geographic and socioeconomic hurdles.
They tackled these challenges by leaning into technology and AI. They deployed AI-powered risk stratification to pinpoint patients with chronic conditions at high risk of hospitalization, enabling proactive care management—reducing avoidable ER visits and admissions by around 10%.
These tech-driven moves paid off hard. In 2023 alone, Geisinger earned over $45 million in value-based care incentives. On top of that, their efforts in population health AI have made real dents in hospitalization and ER rates, while their NLP-powered lung nodule tracking ensures none of those vital findings slip through the cracks.
Value-Based Care Reimbursement Models
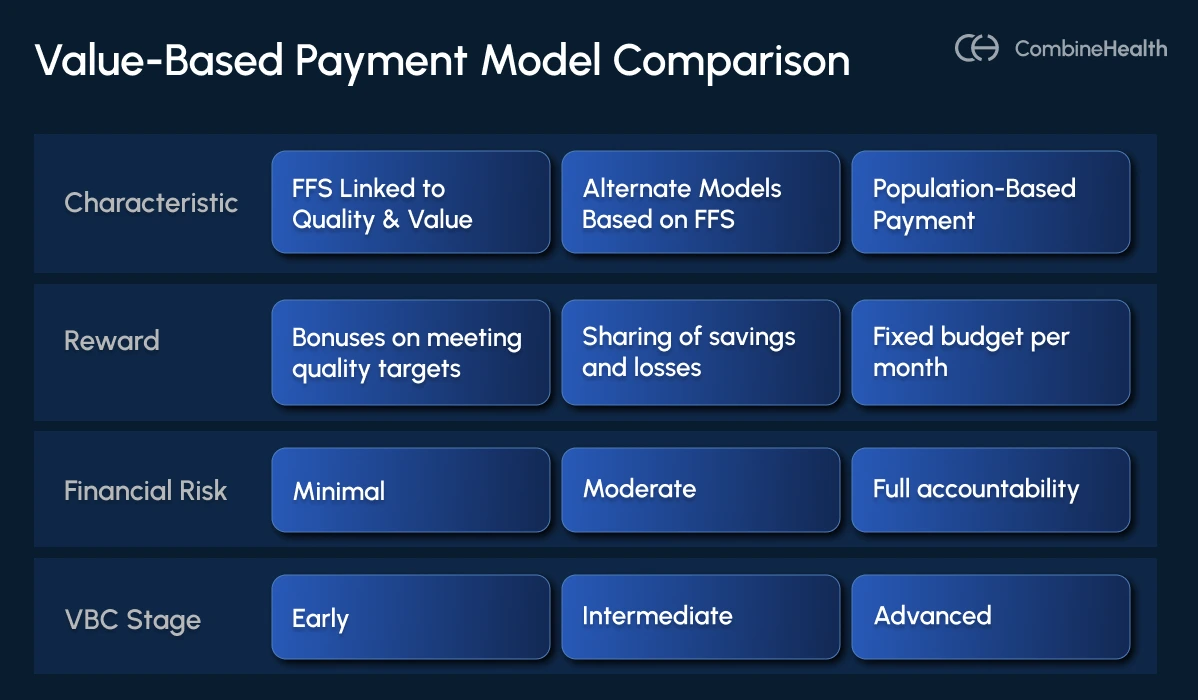
Category 1: FFS with a Link to Quality and Value
This model is still mainly fee-for-service, meaning providers get paid for each service they deliver. However, payments start to connect with how well providers do in terms of quality or reporting.
For example, providers may get bonuses if they report clinical data accurately and on time or meet certain quality benchmarks.
Some popular models are:
Category 2: Alternative Payment Models (APMs) Built on FFS Architecture
This category moves beyond traditional fee-for-service by introducing financial risk-sharing between payers and providers. Providers still get FFS payments as the foundation, but now they can share in both savings and losses based on their performance. This is where many VBC programs are currently positioned.
It includes:
Category 3: Population-Based Payment
This is the most advanced stage of VBC. Instead of paying providers for individual services, payment is based on managing the overall health of a defined population. Providers take on full financial responsibility for delivering coordinated, preventive, and efficient care to that population.
This category includes:
Value-based Care Adoption Challenges
Transitioning to VBC is complex, presenting various challenges alongside significant opportunities.
Data Interoperability
When it comes to value-based care, good data is absolutely essential, especially as AI tools become the secret sauce for smarter, more proactive care.
But here’s the catch: healthcare data is often messy, scattered, and tough to work with.
AI thrives on clean, standardized data, but in reality, data lives in all kinds of formats—fragmented across different systems, incomplete, or even riddled with errors. This is especially challenging when providers try to get a complete picture of a patient’s health for coordinated care.
Then there’s a bigger challenge: Electronic Health Records (EHRs). Many were designed years ago with fee-for-service billing in mind, not for the data-heavy needs of value-based care. So, a lot of that valuable info is buried in unstructured notes, making it tricky to pull out insights that can drive better outcomes.
And it’s not just about the data itself, as:
- Payers can be slow to share data, creating frustrating delays.
- Negotiating access to data can feel like navigating a maze.
- Different formats and definitions mean data often aren’t speaking the same language.
- Care gaps and claims sometimes show up late, making timely intervention difficult.
- Patients hopping between insurance plans can leave gaps in historical data.
All these hurdles mean that, while the promise of AI and analytics in value-based care is huge, getting the right data in the right form at the right time is still a work in progress.
Clinical Relevance and Defined Questions
AI is only as smart as the questions it’s asked to solve. To get meaningful, actionable results, AI algorithms need clearly defined clinical questions.
That’s why it’s critical for clinicians to work closely with data scientists and analysts to identify and refine the key questions AI should tackle, ensuring that insights directly support patient care and clinical decision-making.
Another piece of the puzzle is patient-reported outcomes (PROs)—the feedback patients give about their symptoms, quality of life, and treatment experiences. While PROs can offer valuable insights into care effectiveness, integrating them into clinical workflows can be tricky and time-consuming.
Financial and Operational Complexities
Shifting from the familiar fee-for-service (FFS) model to value-based care (VBC) brings considerable financial and operational challenges. For starters, transitioning isn’t cheap—it often requires significant upfront investments in technology, staff training, and process redesign.
- VBC contracts can be complex to manage due to the wide variety of payment models, quality measures, and contractual terms, which vary by payer and program. This complexity increases administrative overhead and demands sophisticated reporting capabilities.
- Organizations also face financial risks they didn’t encounter under FFS, including costs beyond their control and potential penalties for not meeting performance benchmarks.
- Securing funding for this transition can be tough, especially as the legacy FFS system remains fragile and reimbursement streams are uncertain.
Transition to Value-Based Care with CombineHealth by Your Side
Value-based care is the future of healthcare. But making that future a reality takes more than good intentions. It takes smart tools, clear data, and teams working seamlessly together to put patients first.
That’s exactly where CombineHealth shines.
Our AI agents break down data silos, simplify complex workflows, and deliver insights that help healthcare providers stay ahead of the curve.
By unifying data from multiple sources, we provide a complete patient view that enables accurate risk stratification and helps close care gaps efficiently.
Need to see our agent in action? Book a demo!
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















