Denial Management in Healthcare: An Expert-Backed Playbook for RCM Leaders
Discover proven denial management strategies for healthcare RCM leaders to cut denials, boost revenue, and streamline claims workflows.
August 28, 2025
.webp)

If you deal with denial management in medical billing, you may have heard this somewhere: “86% of claim denials are preventable.”
That’s a big number and a powerful reminder of how much revenue is being left on the table in healthcare organizations every single day.
But you can’t reduce claim denials if you can’t see them clearly, or if they only show up after the money is already stuck in A/R.
That’s where proactive denial management comes in to help you turn a reactive scramble into a repeatable system.
To ground this guide in reality, we sat down with Symone Rosales—a denial leader who lives this every day. Her on-the-ground insights show exactly where denial patterns are shifting, what the common denial causes are, and which denial management moves actually change the numbers.
Key Claim Denial Trends in Healthcare
First-submission denials have become a pattern in recent years.
As confirmed by a survey, denials have been up in recent years. We’re talking about an increase in the volume of denials by 18% from 2020 to 2023, landing around 12% of initial claims getting denied—well above the <5% benchmark.
But what’s pushing denial rates higher? A major force is payer automation.
Insurers are leaning on AI-driven utilization management, which means more stringent checks to ensure more claims stumble on the first try.
We asked Symone about the “why” behind this surge in claim denials, to which she responded:
.webp)
What Are The Common Reasons for Claim Denials?
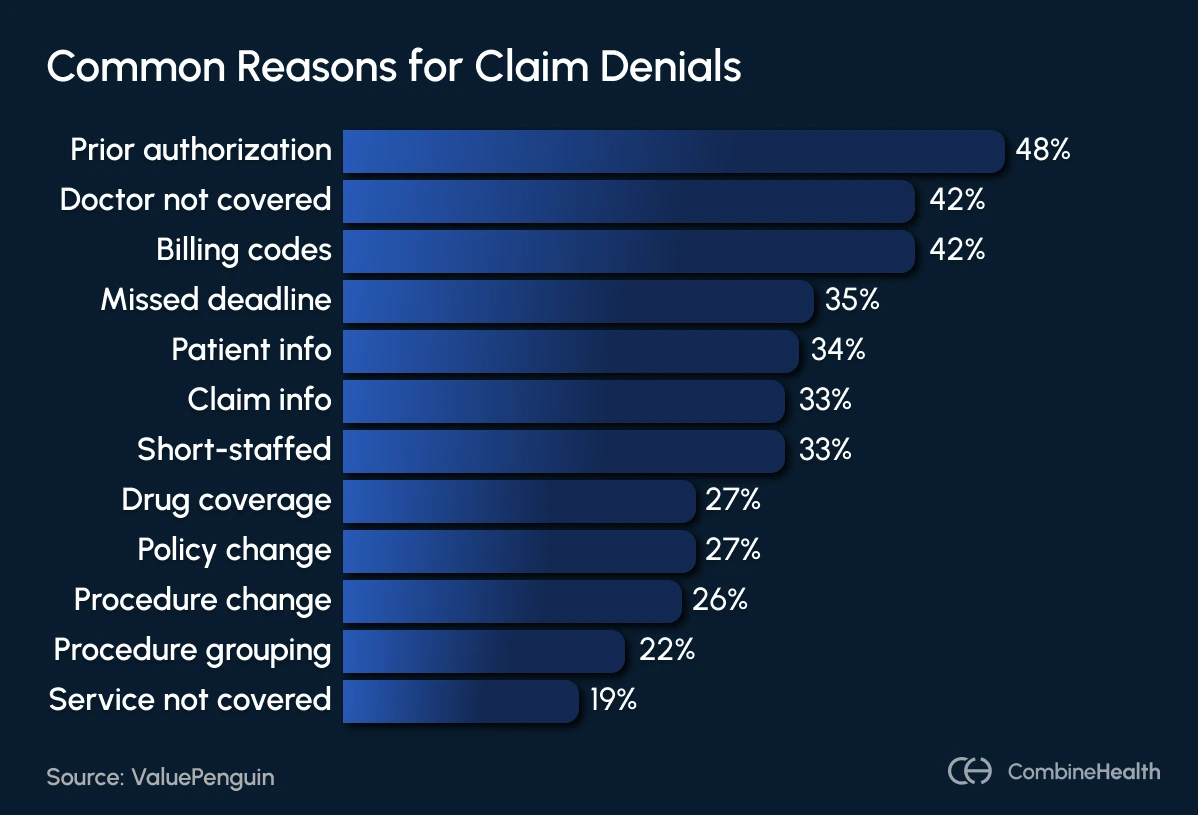
While some claim denials are preventable, others stem from mismanaged RCM teams, overburdened providers, and clumsy claim creation processes.
Excessive documentation requirements for billing and prior authorizations are a constant headache for many providers. Physicians often spend hours on insurer calls, submitting extra details that have little to do with patient care and everything to do with billing.
Labor shortages and high turnover in revenue cycle management (RCM) teams make matters worse. That’s because recruiting and retaining skilled coders and billers is increasingly difficult, and it often leads to backlogs.
Symone shared that their most frequent denial cause was “not being up to date with regulatory changes.” While most claims systems are well built, the cost and manpower required for oversight and maintenance often become barriers.
Outdated technology and poor system integration create further inefficiencies. This involves multiple disconnected billing, coding, and payer portals, which ultimately force staff to work manually across systems. And as a result, this manual hassle increases the “cost to collect” and lowers the first-pass yield.
Some more common frustrations include repetitive denial reasons (like missing info that was actually provided), opaque payer communications, and long phone calls.
A Proactive Denial Prevention Strategy
.webp)
If you ask denial managers what denial issues they keep seeing in their EOBs, you’ll hear the same story: missing authorizations, incorrect patient info, insufficient medical necessity, and coding errors. And yet, every time, it’s the same uphill battle—staff are short-handed, swamped with rework, and unsure how to break the cycle.
But the reality is that many denials can be avoided with proper data, streamlined processes, and a proactive approach.
Symone shared a foolproof denial prevention strategy with us that has helped her cut front-end and back-end denials:
- Stop errors before they hit the claim: Use eligibility and pre-authorization tools at the front end to catch potential issues early on.
- Track every denial: Monitor denial codes regularly. Look for patterns and use root cause analysis to fix systemic issues instead of firefighting one-off claims.
- Fix the big problems first: Tackle high-impact denial categories before anything else. Addressing these will deliver the quickest and most noticeable results.
- Build a central regulatory team: Have a dedicated team to track payer-specific updates and communicate changes rapidly to all stakeholders.
- Create payer scorecards and manuals: Maintain up-to-date manuals with each payer’s top denial reasons, timelines, and appeal strategies. Keep them easy to access across your team.
- Make denial management a team sport: Integrate denial management into multidisciplinary workgroups that include regulatory, coding, billing, CDI, and payer relations. By analyzing denial trends and root causes together, these teams can design systemic fixes that stop repeat issues before they start.
- Anticipate the next denial: Use regulatory insights to proactively adjust pre-bill claim edits before problems arise.
- Integrate payer rules in your tech: Align denial management tools with regulatory feeds so payer-specific rules are built directly into system edits.
At CombineHealth, we give RCM leaders the clarity they need to act fast and wisely.
Our denial dashboards break down performance by month, payer, provider, code, and denial type, so you can see exactly where revenue is leaking and why.
.webp)
KPIs That Prove Your Denial Prevention Strategy Works
Once you’ve rolled out your denial prevention plan, now comes the real test: proving that it’s actually working.
In healthcare RCM, metrics are your secret weapon. And when you track the right KPIs consistently, you shift from reactive firefighting to proactive performance optimization.
Let’s dive into the numbers that not only measure the impact:
.webp)
Symone also shared some golden nuggets of advice for RCM leaders:
- Segment by Payer: Not all payers cause the same kind of denial. Some create more friction or have tougher rules. Segment denial and collection data by payer to laser-target improvement.
- Track Rolling Trends: Use 90-day and 12-month rolling windows. Metrics smooth out and reveal real progress or persistent pain points
- Anchor Ownership: Assign every KPI to a specific owner. When someone’s accountable, things move.
How AI Supports Your Denial Management Process (and Powers Prevention)
Traditional denial management is slow and reactive. But with AI, you switch gears by:
- Automating denial categorization, sorting by payer, provider, or denial type
- Spotting high-impact denials early, so your team can tackle the big revenue risks first
- Assigning denials to the right provider with actionable insights and training
- Uncovering denial trends before they spiral with comprehensive dashboards
Symone shared an optimistic and realistic take on AI’s usefulness in the denial management process:
.webp)
But she also urges caution: misconfiguration is a real risk, and automation done poorly can be a compliance time bomb.
And as an AI-powered RCM workforce vendor, the experts at CombineHealth completely agree with this stand:
.webp)
Here’s what our “human-in-the-loop” approach at CombineHealth entails:
- AI handles the repetitive, time-consuming tasks
- 15% of all charts are flagged for human review to provide oversight, validate outputs, and resolve exceptions
.webp)
This ensures you get the speed and scalability of automation without sacrificing accuracy, compliance, or the nuanced judgment that only skilled professionals can bring.
Proactive Denial Management For the Win!
Denials aren’t random. They tell you exactly where the system needs work.
And from Symone’s insights, it’s clear: most denials are preventable when you shift from chasing fixes to building them in.
By pairing strong processes with real-time data, payer-specific insights, and the right technology, you can stop revenue leakage before it starts.
Curious to know how our AI denial management solution can help? Book a demo with us!
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)









