Healthcare Revenue Cycle Management: Your Blueprint for Fixing Denials and Increasing Collections
A comprehensive healthcare revenue cycle management guide to reduce denials, increase collections, and optimize every stage of the revenue cycle.
December 3, 2025


Key Takeaways:
• Revenue Cycle Management spans every step from appointment scheduling to final payment for the services rendered in healthcare, and small errors in the front end often snowball into denials and payment delays.
• The biggest RCM challenges today include rising denials, changing payer rules, higher operational costs, staffing shortages, and falling patient collections.
• AI now strengthens each stage of the revenue cycle—coding, billing, eligibility, denial management, prior auths—by reducing manual work and preventing errors.
• CombineHealth’s AI agents (Amy, Marc, Adam, Penny, Rachel) automate coding, billing, follow-ups, and appeals with explainability and payer-specific compliance.
• Organizations using AI-driven RCM tools see faster payments, fewer denials, higher collections, and more predictable cash flow—while reducing administrative burden.
A patient comes in, receives great care, you submit the claim, and reimbursement arrives smoothly—the unicorn moment every revenue cycle professional secretly hopes for!
But, in real life, revenue cycle management (RCM) rarely unfolds perfectly. Missing authorizations, reimbursement delays, unexpected denials, and endless administrative back-and-forth can turn a simple revenue cycle workflow into a daily headache.
This is where smarter RCM workflows become your strongest financial safety net. They ensure every dollar you’ve earned actually comes back into your organization.
Let's step inside the RCM world and discover how AI is changing everything.
What Is Healthcare RCM and Why Does It Matter?
Revenue Cycle Management is the step-by-step process that captures every dollar tied to a patient's care. It starts the moment a patient schedules an appointment and ends when you receive the full payment.
Think of RCM as the first domino—even with small inefficiencies and errors, your entire practice feels the impact. Here’s how:
Financial Impact
Most hospitals and medical practices operate under tight margins and rely on a steady cash flow. Even small revenue losses from denials, underpayments, or delayed reimbursements can cause financial setbacks.
For example, suppose a hospital submits 1,000 claims a month at an average reimbursement of $160; even a 10% initial denial rate results in $16,000 in delayed payments. That’s money that could support staffing, supplies, or patient services.
Operational Efficiency
Front-end inefficiencies, such as a typo in registration, a missed eligibility check, or an incomplete chart, can increase claim rework. This drains staff time and reduces productivity.
Similarly, a missed prior authorization can lead to claim denial, delay care, and frustrate patients.
.webp)
Patient Satisfaction
Patient satisfaction may not seem directly tied to the revenue cycle, but it is. Factors that often shape the patient experience include:
- Insurance verification: When insurance coverage details aren’t verified before patient care, patients can be blindsided by surprise bills.
- Communication: Health insurance is confusing for most patients. So when benefit details, out-of-pocket costs, or coverage limitations aren’t clarified, frustration is inevitable.
- Claim delays: When claim processing stalls due to inadequate documentation, coding errors, or slow internal workflows, patients feel the ripple effects. They may receive delayed bills, multiple statements, or unexpected payment requests that catch them off guard.
- Changing payer policies: If changes in insurance rules and reimbursement policies aren’t communicated upfront, patients may face unexpected denials. Unfortunately, from their perspective, the provider is at fault.
Regulatory Compliance
RCM teams juggle a long list of rules from HIPAA, CMS, and various insurance payers. One small misstep can trigger an audit, lead to penalties, or chip away at your reputation.
Take coding, for example. Issues such as upcoding or unbundling—whether intentional or accidental—can result in a post-payment audit. And if auditors find discrepancies, your organization may have to return funds, pay fines, and spend hours cleaning up the issue.
What Are The Steps Involved in Healthcare Revenue Cycle Management?
The healthcare revenue cycle is a detailed, multi-step process involving everyone from your front-desk staff to payers.
Let’s walk you through the RCM workflow step by step:
Hospital-Side Revenue Cycle Process
Healthcare RCM can be divided into three stages: the front end, the mid-cycle, and the back end. Let’s look at each stage one by one:

Front End RCM
1. Scheduling & Registration
This marks the first step of the revenue cycle and the first patient touchpoint. Staff collects essential patient information, including:
- Demographics
- Insurance details
- Medical history
Accurate documentation is crucial, as even a minor typo or missing field can cause eligibility issues and lead to claim rejections.
2. Insurance Verification & Eligibility Checking
Once a patient has registered, the next step is ensuring their insurance actually covers the care they’re about to receive.
During verification, your team confirms:
- Active coverage: Is the patient’s policy valid today?
- Plan type: What's the patient's plan type—PPO, HMO, Medicare Advantage, etc.?
- Benefit details: Are there any deductibles, copays, coinsurance, or benefit limits?
- Authorization or referral requirements: Does the service need prior approval or a referral?
Errors at this stage often lead to denials, such as:
- Inactive or ended coverage: The patient’s plan isn’t active on the date of service.
- Wrong or outdated insurance information: Incorrect member ID, payer details, or plan type.
- No prior authorization: The service required approval, but it wasn’t obtained.
- No referral: The plan required a primary care referral, especially for HMO plans.
- Service not covered: The plan doesn’t cover the procedure or service.
- Benefit limits exceeded: The patient has exceeded the visit limits, therapy sessions, DME allotments, or preventive benefits.
- Out-of-network provider: The provider isn’t in the patient’s network, which can affect coverage.
- Coordination of benefits (COB) issues: The patient has another insurance plan that should be billed as the primary payer.
3. Patient Responsibility & Financial Counseling
In this step, patients learn about their financial responsibility, i.e., their deductibles, copays, and expected out-of-pocket expenses. And today, this conversation carries real weight.
Patient collections have skyrocketed 133% since 2011, and providers often wait more than a month to collect what they’re owed. That makes upfront clarity and transparency essential.
Moreover, the Federal Price Transparency rule now requires providers to share clear, accessible pricing information.
Financial counseling is another vital piece of this stage, especially for patients who may be struggling and requiring financial aid. This step involves helping them understand the costs, exploring payment options, and offering payment plans or financial assistance programs.
Mid-Cycle RCM
Once care is delivered, the focus shifts to clinical documentation and claim preparation.
4. Clinical Documentation
The clinical documentation process starts the moment a patient encounter begins.
The physician documents everything about the encounter: diagnoses, procedures, symptoms, test results, medications, and the care delivered. This documentation becomes the foundation of the medical record and determines what you can bill.
5. Coding & Charge Capture
Once documentation is complete, certified medical coders translate this information into the appropriate medical codes and convert them into charges. This includes:
- Procedures and treatments
- Diagnostic tests
- Medications or injections
- Supplies used
- Follow-up visits or evaluations
Coders translate each service into standardized CPT, ICD-10, and HCPCS codes, reflecting the patient’s condition and the complexity of the services provided.
Some of the most common issues at this stage that could lead to denials include:
- Insufficient documentation for medical necessity: When clinical notes don’t clearly justify the service or level of care provided.
- Upcoding or unbundling: Coding a service at a higher level than documentation supports, or billing bundled components separately.
- Incorrect or mismatched codes/ modifiers: Using outdated codes, selecting codes that don’t align with payer policies, or mismatching CPT and ICD-10 codes.
6. Claim Scrubbing & Submission
After coding, the billing team prepares the claim for submission. But, before a claim is sent to the payer, it goes through a final quality check known as claim scrubbing. This is now widely performed with specialized scrubbing software.
Claim scrubbers review the claim for potential issues such as missing information, documentation gaps, coding errors, or payer-specific rule violations.
If an issue is flagged during the scrubbing process, the claim is held back and routed to the billing team. The billing staff then reviews the edits, corrects coding or documentation errors, adds any missing details or attachments, and follows up with the provider if clarification is needed.
Once corrections are made, the claim is re-scrubbed to ensure accuracy.
Back-End RCM
The back end covers everything that happens after you’ve submitted the claim to the payer.
7. Payment Posting and Reconciliation
Once the payer responds, the billing team records the payments and adjustments in the practice management or billing system. Payment posting involves:
- Entering all payments from insurers and patients
- Applying them to the correct patient accounts and claims
- Recording any adjustments or write-offs from the EOB/ERA
- Updating patient balances based on what the payer has covered
After payments are posted, the reconciliation process begins. This involves comparing the payment received to the reimbursement your practice expects based on contracted payer rates. Reconciliation helps identify:
- Underpayments
- Missing or delayed payments
- Incorrect payer adjustments
- Claims that require follow-up or appeal
8. Patient Billing & Collections
Once insurance payments are processed, any remaining balance becomes the patient’s responsibility. This is where clear communication, transparent billing, and upfront cost estimates at the front end make all the difference.
To improve patient collections and reduce delays, ensure your RCM teams:
- Issue clear, easy-to-understand statements
- Offer multiple payment options
- Provide flexible payment plans
- Maintain open communication
9. Denial & Appeal Management
Despite robust front-end and mid-cycle workflows, claim denials are inevitable. However, what separates ordinary RCM from a high-performing one is how quickly and accurately your team responds when a denial hits.
Denial management is the process of reviewing, correcting, and resolving claims denied by the payer. It typically involves:
- Identifying the reason for denial
- Correcting the issue
- Deciding whether to resubmit or appeal
Appeals are required when the payer denies the claim despite proper documentation or disputes medical necessity. In this case, the provider submits a formal appeal letter along with supporting materials, such as medical records, corrected claim details, progress notes, operative reports, or authorization proof, to justify the claim.
.webp)
10. Financial Reporting
Financial reporting helps you assess the overall health of your revenue cycle.
Key KPIs to monitor your healthcare RCM’s health include:
- Days in Accounts Receivable (A/R): Measures how long it takes to collect payments. High A/R days may indicate slow follow-up, payer delays, or workflow inefficiencies.
- Denial Rate: Tracks the percentage of claims denied by payers. An increasing denial rate often points to issues with documentation, coding, eligibility checks, or prior authorization.
- Clean Claim Rate: Reflects the percentage of claims paid on the first submission. Higher rates mean fewer reworks and faster payments.
- Net Collection Ratio: Indicates the actual revenue collected. A low ratio may signal underpayments, excessive write-offs, or patient collection challenges.
Payer-Side Revenue Cycle Process
Once your billing team submits a claim, it enters the payer’s workflow. While you can’t control how payers operate, insight into their processes helps you optimize your RCM.
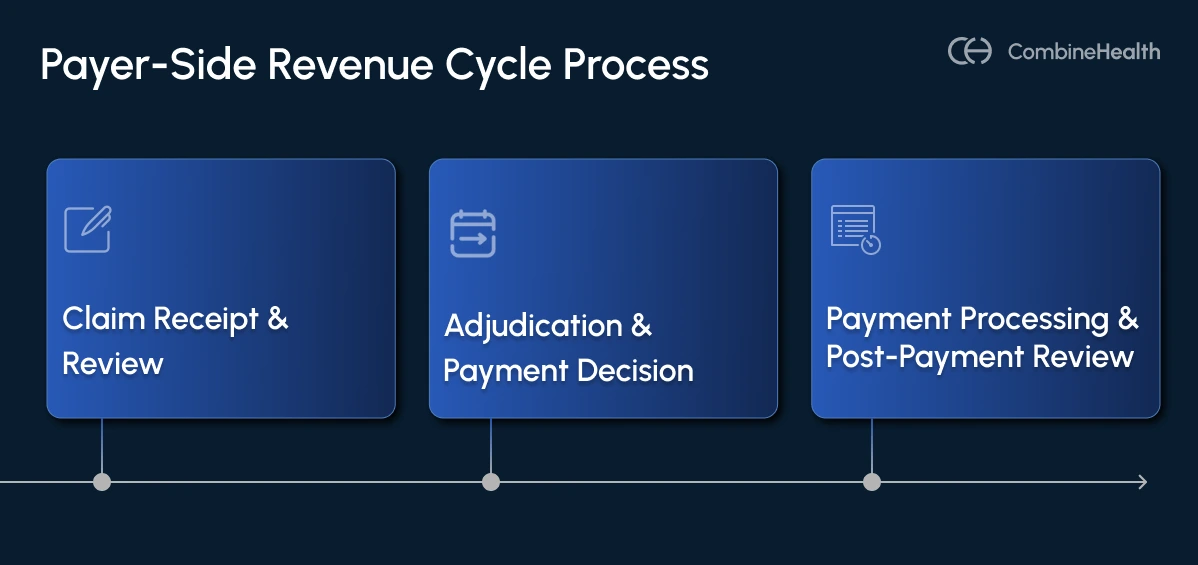
Claim Receipt & Review
When the payer receives a claim, they perform an initial review to ensure all required information is complete and accurate. The payer verifies eligibility, benefits, prior authorization requirements, coding validity, and formatting.
If any information is missing, inaccurate, or doesn’t meet payer requirements, the claim is often rejected immediately.
Adjudication & Payment Decision
After the initial review, the claim moves into adjudication, which is the payer’s formal evaluation process. During adjudication, the payer:
- Applies the member’s benefits to determine what the patient’s insurance plan covers
- Evaluates medical necessity based on clinical guidelines and the patient’s diagnosis
- Checks coding accuracy to confirm that the CPT, ICD-10, and HCPCS codes meet payer-specific coding rules
- Determines the allowed amount the payer will reimburse based on the provider’s contract, fee schedule, and negotiated rates
Once all these factors are reviewed, the payer decides whether to:
- Approve the claim (pay in full)
- Partially pay the claim (due to coverage limits)
- Deny the claim (no payment issued)
Payment Processing & Post-Payment Review
For approved claims, the payer issues payment and documents their decision (along with the reasoning behind it) in an Explanation of Benefits (EOB) or Explanation of Payment (EOP), which is sent to the provider and the patient.
However, payment doesn’t always mean the process is complete. Certain claims, especially high-cost, complex, or high-risk cases, may undergo a post-payment review. This is the payer’s way of ensuring the claim was fully compliant with their policies and that the payment was accurate.
During a post-payment review, the payer may:
- Request additional documentation to verify medical necessity or confirm that services were actually provided
- Adjust the original payment if they determine the billed amount doesn’t match the documentation or coverage criteria
- Recoup funds previously paid if they conclude that services were billed incorrectly or were not medically necessary
What Are The Top 4 Challenges Revenue Cycle Teams Face Today?
Revenue cycle management is becoming increasingly complex, and nearly four in ten medical groups now prefer to outsource or automate parts of the process. Let’s look at the top four RCM challenges:
1. Evolving Payer policies and CPT rules
Providers are struggling to stay compliant with constantly evolving payer policies and coding regulations. As a result, claim denials continue to rise, and nearly half of healthcare leaders now view them as the biggest threat to their revenue cycle.
Simply put, the problem isn’t just persistent; it's getting worse, and RCM teams are spending more time than ever fixing errors and managing appeals.
2. Rising Operational Costs
Healthcare operating costs are also rising, and practices are feeling the squeeze. In fact, 90% of medical practices report higher operating expenses compared to 2024, with labor accounting for 56% of the total hospital expenses, according to an AHA report.
Adding to the pressure, reimbursements aren’t keeping up. The same report mentions that inflation jumped 14.1% between 2022 and 2024, but Medicare payment rates increased only by 5.1%. This gap puts enormous pressure on already-tight margins.
3. Staffing Shortages
Healthcare is facing a serious staffing crisis on both the clinical and administrative sides. And it’s only getting worse. A recent Mercer report projects that by 2028, the U.S. could be short of 100,000 critical healthcare workers and 73,000 nursing assistants.
This workforce crisis is leading to:
- Burnout
- Slower workflows and more backlogs
- Higher turnover and training costs
- Accuracy issues that quickly turn into denial problems
4. Patient Collections
Many RCM teams are finding patient collections harder than ever.
Nearly half of U.S. adults struggle to afford care, and rising patient responsibility makes it even more challenging to collect balances.
For RCM teams, this translates to more follow-up calls, higher aging balances, and lower collection rates.
How AI Is Transforming Healthcare Revenue Cycle Management
Healthcare RCM is intricate, and the maze shifts with every new payer rule and regulatory update. Optimizing RCM manually is tedious.
That’s where AI and automation come in. Here’s how AI RCM is reshaping the future of RCM:
Automating Front-End Tasks
Front-end errors are one of the biggest drivers of denials, and AI helps eliminate them before they ever reach the payer. AI-powered tools can automate:
- Demographic validation
- Insurance verification
- Eligibility checks
- Prior authorization routing
For example, Mark, CombineHealth’s AI billing agent, becomes your front-desk teammate, reducing administrative workload while improving financial transparency and creating a smoother patient experience from the very first touchpoint.
Accurate Coding
Using advanced NLP models, AI interprets clinical documents, extracts structured data, and recommends precise ICD-10, CPT, HCPCS, and E/M codes.
Amy, our AI Medical Coder, reviews encounter notes, assigns the right codes and modifiers, flags documentation gaps, and provides coding rationale in just 2–4 minutes per chart.
With Amy in your team, you achieve:
- Improved coding accuracy
- More complete, compliant documentation
- Faster turnaround time
Efficient Claims Management
Managing claims manually can feel like a juggling act, especially when every payer has its own rules. That’s where AI steps in to take the pressure off your team.
Mark, our AI Billing Agent, automatically applies payer-specific rules, prepares clean, claim-ready charges, checks eligibility, reads ERAs/EOBs, posts payments, and flags underpayments—all without slowing your workflow.
With Mark handling the heavy lifting, errors drop, claims go out faster, and first-pass acceptance rates climb. The result? A smoother, more predictable claims process from start to finish.
Enhanced Denial Management
Denials are rising, yet KFF reports that nearly three-quarters of appealed claims are approved.
Unfortunately, less than 1% of denials are ever appealed, because the process is tedious, time-consuming, and heavily manual. AI resolves this by streamlining and automating the tasks.
For example, Adam, Combine Health’s AI AR & Denial Manager, analyzes denial reasons, navigates payer portals and IVRs, makes AI-driven calls, retrieves real-time statuses, and recommends next steps.
When an appeal is needed, Rachel, our AI Appeals Assistant, drafts payer-specific appeal letters using Amy’s coding rationale and Penny’s policy citations.
Together, they accelerate denial resolution, boost appeal success rates, and prevent avoidable revenue loss.
Improved Compliance
AI makes compliance effortless by staying on top of every payer rule, coding change, and CMS update.
Penny, our AI policy reviewer, ingests every policy update and flags claims that conflict with current requirements. This proactive compliance layer guarantees every claim meets the latest standards, reduces audit risk, and prevents recoupments.
Efficient Decision-Making
AI isn’t just your automation partner, it’s also your advanced analytics assistant.
Taylor, our AI Analyst, consolidates your revenue cycle data into real-time dashboards so you can:
- Analyze denial trends
- Uncover E/M coding insights
- Track key performance metrics
- Pinpoint workflow bottlenecks
- Identify revenue risks before they escalate
With Taylor’s intelligence, you can take swift actions, resolve issues proactively, and drive continuous improvement across your entire revenue cycle.
Must-Have Features to Look for in an RCM Software
You pick the right RCM software, and your finances run smoothly; choose the wrong one, and you’re signing up for nonstop headaches. Here’s a list of features that are non-negotiable in any RCM software:
Some of the non-negotiable features in an Effective RCM Software are highlighted in the table below:
The Future of RCM Is Intelligent, Integrated, and Patient-Centric
Optimizing your RCM is non-negotiable. But you have a choice. You can either do it the hard way, with slow, manual workflows, or the smart way, with intelligent automation and AI guiding every step of the process.
If your goal is to improve financial performance, reduce administrative burden, and future-proof your operations, now is the moment to take action.
Book a demo to explore smarter RCM solutions!
FAQs
1. What is Healthcare Revenue Cycle Management?
Healthcare Revenue Cycle Management is the process that manages all financial and administrative functions from patient appointment scheduling to final payment collection. It ensures providers get paid accurately and on time.
2. What causes claim denials in RCM?
Common reasons include:
- Incorrect or missing patient information
- Coding errors
- Lack of preauthorization
- Late submissions
- Insufficient documentation to justify medical necessity
3. What are RCM KPIs?
Important RCM KPIs include:
- Days in A/R
- First-pass claim acceptance rate
- Denial rate
- Net collection rate
- No-show rate
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















