Clinical Documentation Improvement: Building a Successful CDI Program in Healthcare
Learn what clinical documentation improvement is, why it matters, and how to build a successful CDI program to boost RCM, coding accuracy, and revenue.
December 10, 2025


Key Takeaways:
• Strong CDI programs ensure documentation accurately reflects patient complexity, improving reimbursement and reducing preventable denials.
• Inpatient CDI focuses on concurrent, high-acuity reviews, while outpatient CDI is more retrospective and education-driven.
• The biggest wins of an effective CDI program: cleaner claims, higher CMI, accurate HCC capture, better audit readiness, and faster coding turnaround.
• CDI success requires a defined workflow, the right team (providers, coders, CDI specialists), measurable KPIs, and continuous training.
• AI RCM solutions like CombineHealth's Jessica, Amy, and Taylor help teams scale CDI by capturing complete documentation, reviewing for accuracy, and providing actionable performance insights.
Two providers can deliver identical care, yet walk away with completely different reimbursements.
Ever wondered why that happens?
More often than not, it comes down to one thing: clinical documentation.
CMS reports that nearly 60% of improper payments stem from insufficient documentation. It’s extremely common and surprisingly easy to miss until the revenue is already lost.
That’s exactly why an efficient CDI program matters. It acts like a seal, protecting your practice from preventable revenue leaks.
When a medical record doesn’t clearly capture the diagnosis, the patient’s severity, or the medical necessity behind the service, the claim tells an incomplete story. And an incomplete story may result in lower reimbursement or denials, even when the clinical care was excellent.
That’s exactly where building a solid Clinical Documentation Improvement (CDI) program can help. It helps bridge the gap between the care delivered and what’s captured, ensuring your reimbursement reflects the true complexity of the care.
What Is CDI In Healthcare?
Clinical Documentation Improvement (CDI) or Clinical Documentation Integrity is a process that involves reviewing patient documentation while ensuring it accurately reflects their clinical condition and the care delivered.
A CDI specialist typically reviews:
- Diagnoses to confirm they are complete, specific, and clinically supported
- Treatments to ensure the medical necessity is clearly documented
- Clinical indicators, i.e., labs, imaging, vitals, and progress notes that validate the clinical picture
- Hospital-acquired conditions (HACs) to ensure accurate reporting and compliance
- Procedure details, including laterality, approach, and key findings
- Discharge summaries to verify final diagnoses and the overall course of care

How Does a CDI Program Work?
The workflow in a hospital (inpatient) differs significantly from that of a private practice (outpatient). Here’s how:
CDI in an Inpatient Setting
Inpatient CDI is more complex due to higher acuity, longer stays, DRG-based billing, and extensive quality reporting. It typically involves:
- Case Prioritization: Flagging high-risk diagnoses and complex cases
- Concurrent Review: Reviewing documentation for specificity, completeness, and accurate capture of severity and complications, while the patient is still admitted
- CDI Queries: Sending standardized queries when documentation is unclear or incomplete
- Provider Updates & Education: Providers clarify documentation; CDI teams reinforce best practices and compliance expectations
- Coding & Billing: CDI and coding teams reconcile DRGs to prevent DNFB delays, denials, and billing issues
- Monitoring & Reporting: Tracking CMI metrics for ongoing optimization
CDI in An Outpatient Setting
Outpatient CDI is mostly retrospective, often reviewed days or weeks after the visit. It includes:
- Documentation Review: Identifying missing specificity, weak E/M support, poor medical necessity, and uncaptured chronic conditions
- Provider Education: Offering actionable feedback to improve diagnosis specificity and chronic condition documentation
- Proactive Improvement: Most corrections occur at the next visit, where providers refine the clinical narrative
- Audits: Reviewing E/M levels, HCC capture, medical necessity, and denial trends to refine templates and workflows
What Are the Benefits of a CDI Program?
A robust CDI program does more than refine documentation. Here’s what it brings to the table:
- Accurate Coding: Clear, specific documentation supports correct ICD-10, CPT, DRG, and HCC coding.
- Higher Reimbursement: When documentation accurately reflects patient complexity, payments align more closely with the care delivered.
- Fewer Denials: Meticulous clinical details prevent denials due to medical necessity, coding errors, and inadequate documentation.
- Better Audit Protection: Complete documentation helps defend against RAC (Recovery Audit Contractors), MAC (Medicare Administrative Contractors), and payer audits.
- Improved Quality Metrics: Accurate documentation boosts CMI (Case Mix Index), risk adjustment scores, and publicly reported quality outcomes.
- Stronger Care Coordination: Clear records improve communication across teams and reduce clinical errors.
- Operational Efficiency: Cleaner documentation accelerates coding, eliminates billing delays, and streamlines workflows.
Steps to Create an Effective CDI Program
When creating a CDI program, simply hiring a CDI specialist doesn’t solve the problem.
What you really need is a structured strategy; one that brings the right people together, follows standardized workflows, and is supported by the right technology.
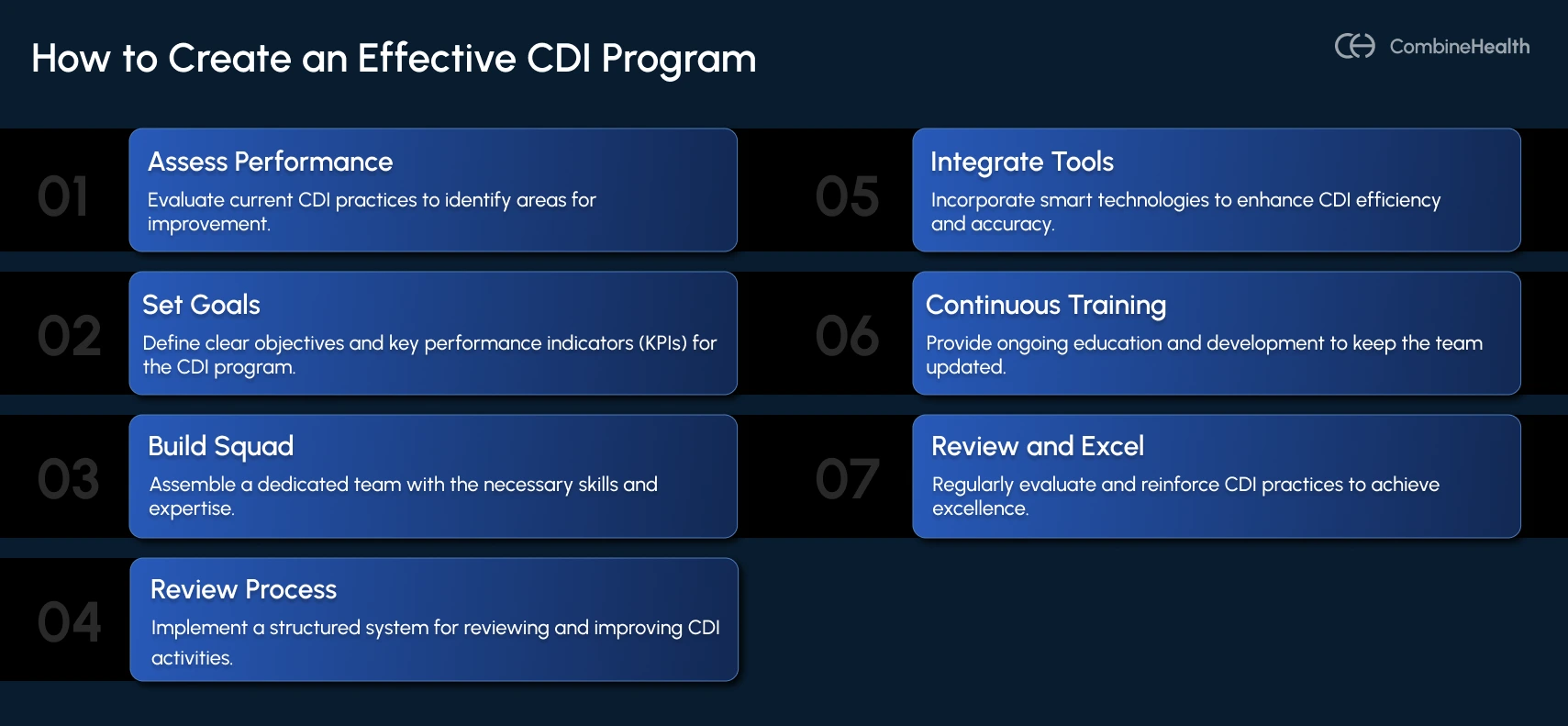
Here’s a practical, easy-to-follow roadmap for building a CDI program that’s efficient, scalable, and built for long-term success.
1. Assess Your Current Documentation Workflows
First, evaluate your current documentation practices. A baseline assessment can reveal gaps that need attention and opportunities for improvement.
Focus your review on these areas:
- Chart documentation quality
- Coding accuracy patterns
- Denials tied to medical necessity or insufficient documentation
- Quality metrics
- Chronic condition capture (for HCC/RAF models)
- Specialties and service lines with the most risk or financial impact
- Payer-specific denial trends
This baseline becomes your reference point for measuring CDI performance over time.
2. Establish Clear Goals and KPIs
Once you've identified your documentation gaps, the next step is turning those insights into measurable goals. Make sure your goals are specific, realistic, and tied to KPIs so you can track progress over time.
Here’s what clear, metric-driven CDI goals should look like:
- Increase documentation-related denial resolution by 20% in six months
- Improve CMI by 0.05 within one year
- Increase chronic condition (HCC) capture accuracy by 25% within the next reporting cycle
- Reduce DNFB days to 3 days per case or less
- Reduce medical-necessity denials by 30% in the next six months
3. Build Your CDI Operations Squad
An effective CDI program is a team effort, for which you'll need a task force with diverse expertise.
Form the right mix of CDI squad that includes:
- Physicians or Physician Advisors who provide clinical validation, clarify diagnoses, and support timely query resolution.
- Certified coders who accurately apply ICD-10, CPT, DRG, and HCC codes and make sure the coding meets billing and compliance standards.
- CDI Specialists who review charts, identify documentation gaps, craft queries, guide providers on documentation best practices, and ensure regulatory compliance.
- Practice Managers who oversee financial impact, monitor denial trends, track CDI-related KPIs, and ensure alignment with revenue cycle goals.
4. Establish a Structured Review Process
Once your CDI squad is in place, the next step is building a clear, standardized CDI workflow. This ensures everyone follows the same playbook and the CDI process is consistent across the organization.
Your CDI playbook should outline guidelines for:
- Chart Prioritization: Identify which cases should be reviewed first, such as high-risk diagnoses, complex encounters, or payer-sensitive cases.
- Query Creation, Routing, and Tracking: Standardize how queries are written, where they’re sent, and how responses are tracked to ensure nothing slips through the cracks.
- Post-Query Follow-Up: Clarify who updates the documentation, how disagreements are resolved, how coding is adjusted, and how completed cases are closed.
- Handling Non-Responsive Providers: Set clear query response timelines and define escalation steps if they remain unanswered despite reminders.
- Quality Assurance (QA) Checks: Conduct regular audits to review query quality, ensure documentation consistency, and strengthen collaboration between the stakeholders.
5. Integrate Smart Tools Into Your CDI Process
A smart way to accelerate CDI success is to make technology your ally. Integrating the right solutions at each stage enhances efficiency and lightens the administrative load.
Here are some tools that boost CDI performance:
- Smart EHR Templates: Standardize documentation by prompting for critical details like acuity, laterality, and diagnostic specificity
- AI Medical Scribes: Convert provider–patient conversations into accurate, structured clinical notes in real time
- AI-Driven Chart Review (NLP): Scan records to flag missing specificity, unsupported diagnoses, and overlooked comorbidities before billing
- CDI Software: Streamline the entire query workflow with automated creation, routing, tracking, reminders, and escalations
- Automated Coding Solutions: Assign ICD-10, CPT, E/M, DRG, and HCC codes while identifying gaps and accelerating coding turnaround
- Predictive Analytics & Dashboards: Prioritize high-impact charts and provide real-time visibility into CDI and RCM performance metrics
6. Fortify Your Squad With Continuous Training
With new regulations, coding updates, payer policies, and documentation requirements evolving, ongoing CDI training becomes your greatest advantage.
Offer role-specific, targeted training that keeps everyone in your task force aligned and up to date.
- For Physicians: Offer training for documenting high-impact conditions (e.g., sepsis, heart failure, COPD, malnutrition) and highlight the direct impact this has on reimbursement, CMI, HCC accuracy, and quality reporting.
- For Coders: Offer refreshers on ICD-10, CPT, HCPCS, and HCC changes, plus the payer rules that influence E/M and risk adjustment. Reinforce coding practices around specificity, proper sequencing, and audit readiness.
- For CDI Specialists: Ensure their expertise is aligned with current documentation standards, AHIMA/ACDIS guidelines, CMS/OIG audits, and evolving payer policies.
7. Review, Reinforce, and Excel
Improvement doesn’t stop once your CDI program goes live. Keep an eye on your core CDI KPIs so you can refine workflows, sharpen templates, refresh training, and support your team. This continuous refinement is what drives long-term program success.

What are the Metrics That Define a Successful CDI Program?
Creating a CDI program sets the foundation; measuring its performance is what makes it thrive. Here are the key metrics that define CDI success:
How Combine Health’s AI Agents Boost Your CDI Performance
We’ve discussed the role of technology in CDI, but AI solves a more immediate challenge: bandwidth.
According to an HFMA survey, 53% of healthcare leaders expect CDI roles to be the hardest to staff over the next three years. The same report notes that 26% struggle with denials and documentation improvement due to tech gaps and poor coordination between clinical and RCM teams.
AI helps close these gaps by acting as a smart scribe and reviewer—lightening the workload, improving documentation accuracy, and ensuring consistency. Best of all, it allows practices to maintain CDI quality even without a fully staffed CDI team.
Here’s how Combine Health’s AI agents step in to support your CDI efforts.
Jessica: Your Real-Time AI Medical Scribe
Documentation shouldn’t take over your day, and with Jessica, it doesn’t. Just speak naturally during the patient visit, and she captures everything in real time.
Jessica turns the entire conversation into clean, accurate clinical notes, progress notes, SOAP notes, or visit summaries, all neatly structured and ready for the EHR. And because she understands specialties like cardiology, orthopedics, primary care, and more, the documentation always reflects the details payers look for.
How Jessica helps providers:
- Reduces documentation burden by letting providers spend less time on screens and more time engaging directly with patients
- Ensures comprehensive documentation by capturing the full patient–provider conversation through the speech-to-text feature
- Accurately records the medical history, Review of Systems (ROS), and the assessment
- Captures key clinical indicators and specialty-specific details such as laterality, acuity, and stage
- Improves accuracy by documenting everything in real time, reducing the risk of missing information
Amy: Your AI Coding & Documentation Review Assistant
Once the note is ready, Amy steps in to handle the coding heavy lifting. She reviews the encounter, suggests the right CPT, ICD-10, E/M levels, and modifiers, and — unlike most AI tools — explains exactly why she picked each code. No black boxes, no guesses.
Amy also spots documentation gaps that could cause denials later, like missing clinical indicators or incorrect diagnosis sequencing. With her 2–4 minute review time and ability to process charts in parallel, your team gets both speed and accuracy without the extra workload.
How Amy helps your team:
- Speeds coding workflows by giving coders pre-reviewed charts with suggested codes and a clear rationale behind each choice
- Reduces rework by flagging missing elements such as specificity (e.g., type of pneumonia), acuity, time documentation for prolonged services, or laterality for specialty-related cases
- Provides feedback to physicians when documentation doesn’t fully support a diagnosis, E/M level, or procedure, making improvements simple and immediate
- Prevents denials by identifying potential payer risks early, improving your clean claim rate
Here's a quick example of Amy in action:
Suppose after a patient encounter, a provider documents: “Type 2 diabetes, on insulin.”
Amy reviews the chart and notices additional information already in the record—an A1c of 10.5 and neuropathy symptoms—that isn’t reflected in the provider’s note.
She offers a gentle, context-aware prompt:
“The patient appears to have poorly controlled type 2 diabetes with diabetic neuropathy. If accurate, consider documenting this.”
With that reminder, the provider updates the note to:
“Poorly controlled type 2 diabetes with diabetic neuropathy, on insulin.”
The documentation now includes the level of specificity required for accurate coding. Based on the updated note, Amy suggests the appropriate ICD-10 codes—E11.40 (Type 2 diabetes with diabetic neuropathy) and Z79.4 (long-term use of insulin)—and recommends an E/M level that aligns with the documented clinical complexity.
Taylor: Your CDI Performance Analyst
You may have a wealth of data, yet converting this information into meaningful, actionable insights is often a challenge.
No worries; just ask Taylor, and you’ll get the insight you need in a clean, ready-to-use dashboard. You can simply ask Taylor, “What documentation issues are we running into?” or “Which queries are taking the longest to resolve?” and Taylor gives you instant, actionable answers.
How Taylor helps you:
- Reveals documentation patterns, such as frequently missed diagnoses or incomplete assessments, so you know exactly where improvement is needed
- Identifies coding issues by highlighting recurring problems like incorrect modifiers, under-coded services, or documentation gaps that slow down turnaround time
- Delivers real-time CDI analytics by tracking query response rates, documentation completeness, and high-impact diagnosis trends
Together, Jessica, Amy, and Taylor create a complete AI-powered CDI task force that supports every step of documentation, coding, and revenue integrity. This teamwork reduces the workload on providers, coders, and CDI specialists.
Accelerate CDI Success With a Smart AI Task Force
The healthcare workforce crunch and regulatory shifts aren’t passing storms; they’re long-term realities that may intensify before they improve. In a landscape this demanding, manual CDI processes are no longer sustainable. Your practice needs support that’s fast, accurate, and scalable—and AI is the only solution that can consistently deliver at that level.
The next era of CDI belongs to teams that embrace intelligent automation. Don’t let your organization fall behind in this competitive race.
Ready to elevate your CDI program? Let’s connect and build the future of documentation together.
FAQs
What is Clinical Documentation Improvement (CDI) in healthcare?
CDI is a structured process that enhances the accuracy, completeness, and specificity of clinical documentation, so the medical record reflects patient severity, services provided, and clinical outcomes. This supports high-quality care, accurate coding, and compliant reimbursement.
How does CDI impact revenue cycle management (RCM)?
CDI strengthens RCM by reducing documentation-related denials, improving DRG and HCC accuracy, streamlining coding and billing, and ultimately increasing net revenue and cash flow.
What documentation gaps commonly hurt reimbursement?
Denials due to inadequate documentation occur due to vague or missing diagnoses, unspecified severity or laterality, incomplete comorbidity capture, conflicting provider notes, and diagnoses not supported by labs, imaging, or exam findings.
What is the role of a CDI specialist?
A CDI specialist reviews charts for specificity and clinical completeness, issues queries when clarification is needed, partners with coders, and educates providers on documentation practices that support accurate coding, quality reporting, and appropriate reimbursement.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










