How To Appeal an Insurance Claim Denial: A Provider’s Guide
Discover the step-by-step process for appealing denied insurance claims and understand when a corrected claim is better than an appeal.
August 30, 2025


Key Takeaways:
• Not every unpaid claim is an appeal; start by distinguishing rejections, reopenings, reconsiderations, and true denials.
• Decoding CARC/RARC codes on the EOB/ERA is the first step to knowing the right path forward.
• Strong appeals rely on complete documentation packets that directly match coverage criteria.
• Correctable errors should be fixed with a corrected claim to avoid unnecessary appeals and speed payment.
• AI-powered tools like CombineHealth’s AI Agents can streamline appeals, reduce manual effort, and improve overturn rates.
Denials are a huge part of the revenue cycle management process.
Appeals, though necessary, often feel like they drain more time and energy than they return. Teams sift through EOBs, chase down documentation, and draft letters under tight deadlines.
For hospital leaders, the challenge isn’t just overturning one denial. It’s building a repeatable process that keeps cash moving and prevents revenue from slipping through the cracks.
This guide walks through a step-by-step approach to filing insurance claim denial appeals effectively and how AI can help lighten the load along the way.
Before You Start: Is It a Rejection, or a Denial?
One of the easiest ways to waste weeks in A/R is by working a claim in the wrong lane. For that, you must be able to distinguish between rejections and denials.
A rejection happens before adjudication and during clearinghouse edits or front-end payer checks. These claims never make it into the payer’s system, which means they carry no appeal rights.
The fix is straightforward: correct the data (subscriber ID, DOB, coding format, NPI, etc.) and resubmit.
.webp)
A claim denial, on the other hand, occurs after adjudication. The payer has processed the claim, issued an ERA/EOB, and explicitly decided not to pay, citing a CARC/RARC reason code. Denials are what trigger the formal appeal process.
Reopening vs Reconsideration
For Medicare claims, there are two additional lanes worth knowing: Reopening and Reconsideration.
A reopening is basically Medicare’s way of letting you fix small clerical mistakes without going through the entire appeal process. Think of things like a typo in a code, a wrong date, or a simple math error. In those cases, you can ask the Medicare Administrative Contractor (MAC) to reopen and correct the claim, and it’s usually quicker than filing an appeal.
A reconsideration comes into play only if you’ve already gone through the first step of the Medicare appeal process (a redetermination) and the denial still stands. At this stage, the case gets sent to a qualified independent contractor (QIC) for a fresh review.
The Step-by-Step Denial Appeal Process
Denial appeals work best when they follow a clear, repeatable process. From reviewing the EOB to assembling records and drafting the appeal, each step builds the case for payment.
Here’s how to approach denial appeals in your organization:
Step 1: Dig Through the EOB/ERA to Decode the “Why”
Every denial comes with an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA), an official document from the payer stating why the claim didn’t get paid. This is communicated in the form of Group Code, CARC (Claim Adjustment Reason Code), and sometimes an attached RARC (Remittance Advice Remark Code).
Example:
CO-50: “Not medically necessary"
CO-109: “Claim not covered by this payer/contractor”
CO-18: “Duplicate claim/service”
According to CMS and the X12 code set, the CARC/RARC combo is the only standardized language you’ll get from the payer. If your team doesn’t decode it correctly up front, you risk sending the wrong appeal, and that can cost weeks in A/R and put dollars permanently at risk.
Recommended Reading: Common claim denial codes and what they each mean
Step 2: Identify the Denial Reason Precisely
Once you’ve decoded the EOB/ERA, don’t stop at the surface code. A CO-50 (“Not medically necessary”) on its own doesn’t tell you what the payer really wants.
To move an appeal forward, you need to map the denial back to the exact policy language or coverage criteria the payer is applying:
- Medicare claims: Check the relevant National Coverage Determination (NCD) or Local Coverage Determination (LCD). These outline the covered diagnoses, documentation standards, and clinical benchmarks Medicare uses to approve or deny payment.
- Other health plans: Most insurers publish coverage policies that define what they consider medically necessary. Look up the procedure or diagnosis to see what documentation, prior authorization, or clinical history is required.
Step 3: Pull Clinical Records & Evidence
Once you’ve pinpointed the denial’s root cause, your next move is building a documentation pack that makes reversal almost inevitable.
This pack should include:
- Physician’s notes containing evidence that the service was formally ordered and medically connected to the patient’s condition
- Diagnostic reports, including lab results, imaging, or pathology, tied directly to the billed service
- Prior authorization proof, including faxes, approval codes, or portal screenshots showing clearance when applicable
- Coding rationale aligning diagnoses with procedure codes
Step 4: Send Corrected Claim (If Applicable)
Not every denial needs to follow the lengthy appeal pathway. In many cases, what looks like an “appeal” situation is actually a correctable error that can be resolved faster by sending a corrected claim.
Commercial payer UnitedHealthcare clearly outlines the difference: if you need to correct the date of service or add a modifier due to a billing error, you should submit a corrected claim, not an appeal.
Here’s when to go for correction:
- Demographic errors: Patient DOB, subscriber ID, or gender mismatch.
- Clerical/coding typos: Wrong modifier, transposed digits in a CPT/ICD code.
- Billing edits: Missing NPI or taxonomy mismatch flagged by the payer.
- Duplicate submissions: Same claim billed twice under different dates or lines.
Step 5: Write the Formal Appeal Letter
Once you’ve decoded the denial, confirmed it’s not just a correction, and assembled your clinical evidence, the next move is drafting the appeal letter. This is where your denials team takes the raw data and turns it into a persuasive case.
Here’s what every appeal letter should contain:
- Administrative header: Patient name, date of service, claim number, denial code, provider name/NPI, and contact information, statement of what you’re requesting
- Information about the denial: Quote the exact denial language from the EOB/ERA and cite the corresponding payer policy
- Clinical narrative: Summarize the patient’s condition, clinical decision-making, and failed conservative measures
- Supporting evidence: List attachments: physician notes, operative reports, test results, prior auth records, and relevant policy excerpts
- Closing statement: Respectful but firm ask for claim payment based on the evidence presented
Useful Resource: A set of denial appeal letter templates from ACEP
What Does AI-Powered Denial Management Look Like?
Managing denials has traditionally been one of the most manual and resource-heavy parts of revenue cycle management. Teams spend hours combing through payer policies, pulling records, drafting letters, and tracking deadlines, often under tight filing windows.
AI is changing this narrative by reducing turnaround times and allowing denial teams to focus their expertise where it matters most. AI tools can now:
- Draft appeal letters
- Reference payer policies
- Track filing limits
- Follow up with payers through portals or phone systems
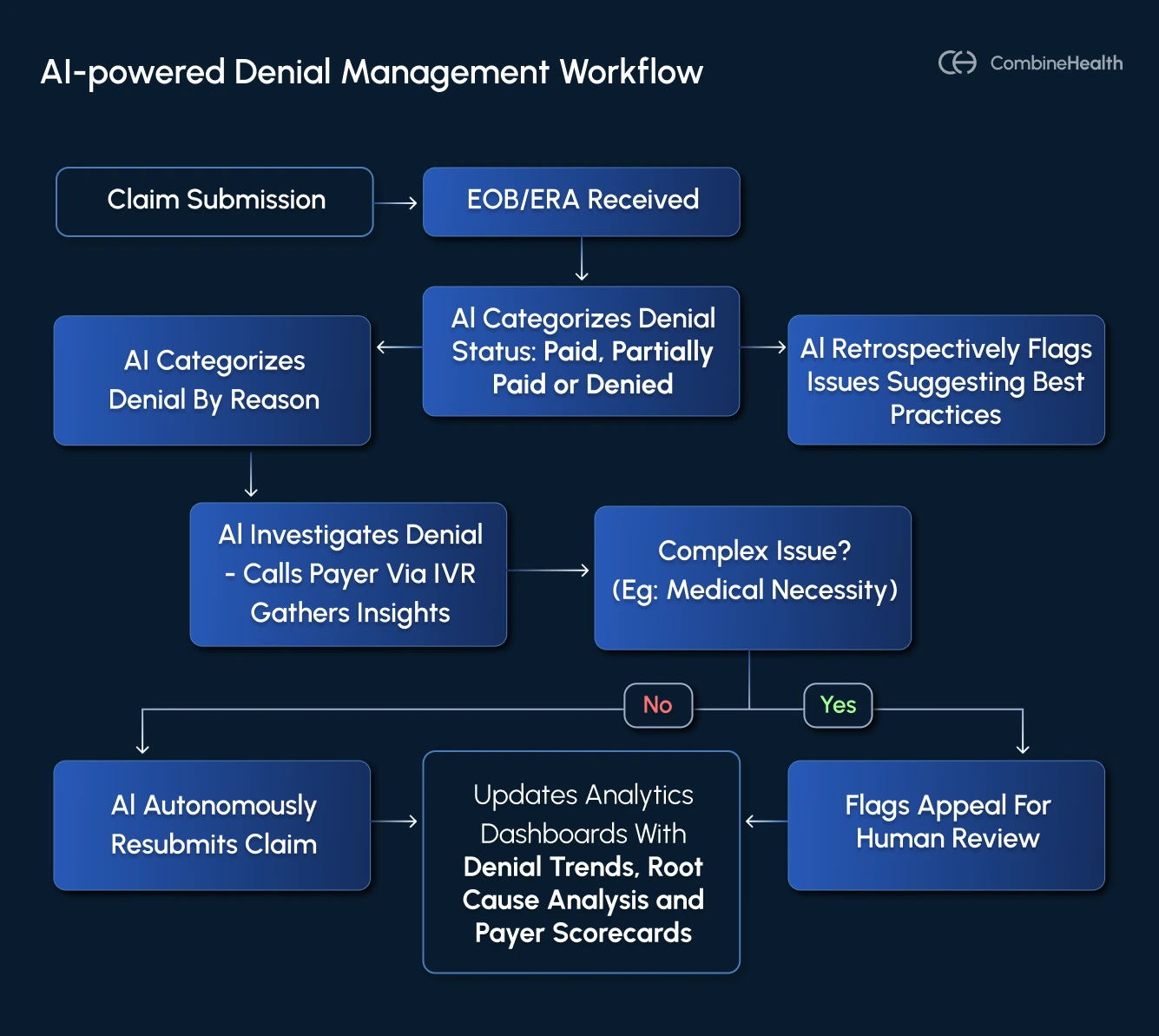
CombineHealth’s AI Denial Agents To the Rescue!
At CombineHealth, the claim appeal work is supported by a coordinated set of AI agents:
- Rachel (AI Appeals Assistant) generates clear, payer-specific appeal letters backed by coding rationale and policy citations.
- Adam (AI Denial Management Agent) works denials through portals and calls to gather status updates and escalate when needed.
- Penny (AI Policy Reviewer) surfaces the exact coverage criteria or medical necessity guidelines tied to each denial.
- Taylor (AI Revenue Cycle Analyst) provides visibility into patterns, helping leaders prioritize high-value appeals and spot upstream fixes.
Together, these tools help RCM leaders shift appeals from a reactive, manual burden to a streamlined, data-driven process.
Want to see them in action? Book a demo!
FAQs
What is a denial appeal?
A denial appeal is a formal request for a payer to review and overturn their initial decision not to pay a claim.
How long do I have to appeal a denied claim?
Timelines vary by payer, but most commercial health plans give providers up to 180 days from the date of denial to file an appeal.
What happens when you appeal a denied claim?
Once submitted, the payer reviews your appeal packet, which usually includes a letter, clinical records, and any policy references.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










