Modifiers in Medical Billing: How AI Simplifies Their Use in Revenue Cycle Management
Learn what modifiers in medical billing are (including modifier 25, 59, 26, 76), why they matter for reimbursement, and how AI can simplify modifier management in RCM.


Key Takeaways:
• Modifiers in medical billing are appended two-digit codes that explain special circumstances of a service without changing its definition.
• Use-cases: modifier 25, modifier 59, modifier 26, 76 modifier, JW modifier, XS modifier, among many.
• Accurate use of modifiers directly affects reimbursement, claim denials, AR days, and audit risk.
• Why we use modifier 25 in medical billing: to bill an E/M service when performed separately from a procedure.
• Using modifier 59 vs X-modifiers in medical billing: X-modifiers (XE, XS, XP, XU) often provide more specificity and may reduce audit risk compared to 59.
• AI-driven RCM tools can detect incorrect modifier use before submission, automate documentation matching, and help you recover lost revenue.
Revenue cycle teams know the drill: a claim hits the payer, it pays—but then it gets denied, underpaid, or flagged because of a modifier in medical billing that was missing, incorrect, or misplaced. In many practices, this means hours of review, appeals, and frustrated staff.
That’s because billing teams handle hundreds of claims each week, and even small modifier errors can trigger audits, manual reviews, and lost revenue.
This article walks you through the importance of modifiers in medical billing and the common types that are used in RCM processes today. You’ll also explore how AI can help with modifier management and keep modifier-related denials to a minimum.
What Are Modifiers in Medical Billing?
Modifiers are two-digit numeric or alphanumeric codes appended to a CPT or HCPCS code. Their purpose is to indicate that a medical procedure or service was altered by specific circumstances without changing the fundamental definition of the service itself.
Example:
If a patient undergoes a distinct procedural service on the same day as an unrelated evaluation, modifiers help justify separate billing and payment.
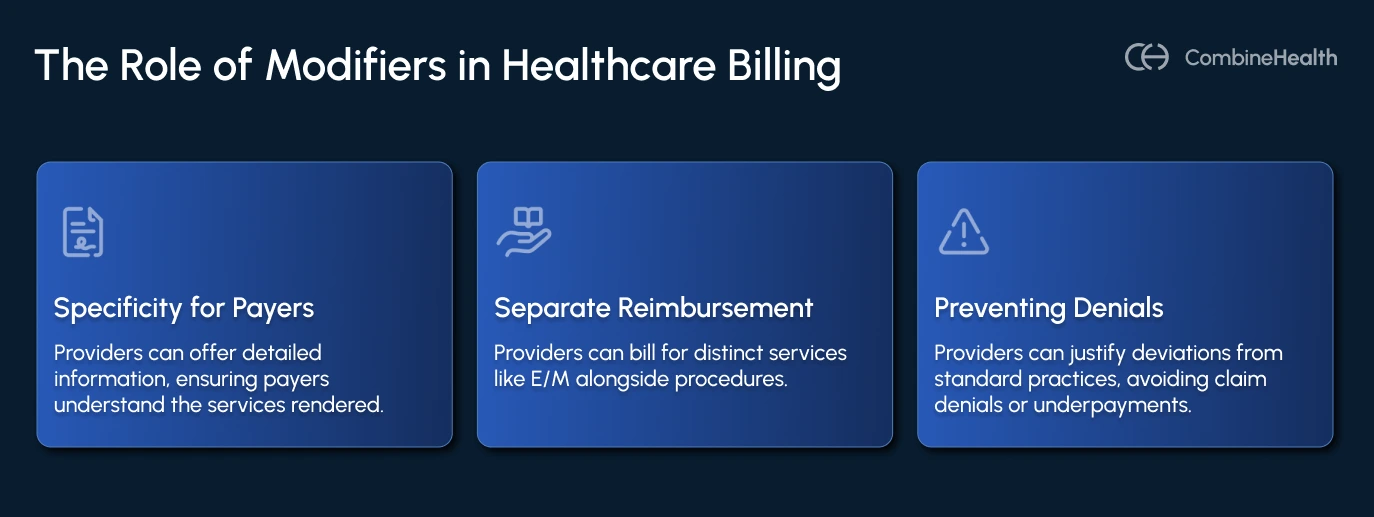
They help healthcare providers in:
- Providing more specificity so payers understand exactly what happened
- Enabling separate reimbursement when appropriate, such as billing an evaluation and management (E/M) service alongside a procedure
- Preventing denials or under-payments by explaining why a service differs from the norm
Common Scenarios Requiring Modifiers
Modifiers are essential in numerous real-world situations encountered by healthcare professionals, which involve the following cases
- When a patient receives a separately identifiable evaluation and management service (E/M) on the same day as a minor procedure performed by the same physician, modifier 25 is used to bill both services distinctly.
- For diagnostic tests that include professional and technical components, such as imaging studies, modifier 26 allows billing for the professional component only.
- When two distinct procedures are performed on different lesions or organs by the same provider on the same day, modifier 59 or its HCPCS level II variants clarify the distinct procedural service.
- If the same physician performs a repeat procedure later on the same day, modifier 76 indicates this repeat service.
Types of Modifiers in Medical Billing
Modifiers primarily fall into two categories: CPT modifiers (level I) and HCPCS modifiers (level II).
They can also be classified as pricing modifiers, which affect reimbursement, and informational modifiers, which provide additional context but do not directly alter payment amounts.

Below is a table listing some commonly used modifiers with their type and typical use:
This list is part of a comprehensive catalog of modifiers widely used in medical billing, which includes over 70 recognized modifiers. The correct use and understanding of these modifiers are essential for compliance and proper reimbursement.
CPT and HCPCS Modifiers
Modifiers are appended to CPT codes (used for describing medical procedures and services) and HCPCS Level II codes (cover items, supplies, and services not included in CPT).
Some examples include:
- Numeric two-digit modifiers such as 25, 59, and 26
- Drug wastage modifiers like JW and JZ
- Distinct procedural service variants of modifier 59, including XE, XS, XP, and XU
Pricing vs Informational Modifiers
Pricing modifiers indicate altered billing or reimbursement circumstances (e.g., 26, 59, 76) and they directly impact the payment amount. Informational modifiers, on the other hand, provide extra detail but don’t change base payment (e.g., LT/RT laterality, 33 for preventive services) and usually have no effect on the payment amount.
Functional modifiers should typically occupy the first modifier position, followed by informational ones to avoid confusion or claim rejection.
Example:
Suppose a provider performs a diagnostic X-ray of a patient’s left knee and bills only for the professional component (the physician’s interpretation). In this case, modifier 26 (professional component) is the pricing modifier, and modifier LT (left side) is the informational modifier.
The correct claim line order would be:
CPT 73560-26-LT → X-ray of knee, professional component only, performed on the left side.
Here, modifier 26 appears first because it affects how the claim is paid, while modifier LT comes second since it provides additional information without altering payment.
Key Modifiers RCM Leaders Must Know
Here is a short list of modifiers and when to use them in your medical billing process:
- 25 modifier in medical billing: Indicates a significant, separately identifiable evaluation and management service on the same day as another procedure.
- 59 modifier in medical billing: Denotes a distinct procedural service unrelated to other services performed that day; used only when no more specific modifier applies.
- 26 modifier in medical billing: Represents the professional component of a service, separating it from the technical component.
- 76 modifier in medical billing: Used for repeat procedures or services performed by the same provider on the same day.
- JW modifier in medical billing: Indicates drug amount discarded/waste indicator.
- XS modifier in medical billing: Specifies a separate structure distinct service; variant of 59.
Why Modifier Accuracy Matters for RCM Leaders
Many RCM leaders struggle with growing accounts receivable, recurring denials, and underpayments that can often be traced back to modifier misuse. The problem extends beyond isolated claims; incorrect modifier use can lead to widespread revenue leakage, increased appeals workload, and heightened audit risk.
When modifiers are applied incorrectly—for example, using modifier 59 instead of 76, or omitting modifier 25 when billing an E and M service alongside a procedure—the consequences extend beyond a single claim. Each mistake can result in reduced payments, additional appeals, or even audit flags. When this pattern repeats across thousands of claims, the cumulative effect leads to significant revenue leakage and heightened compliance risk.
Impact on Reimbursement, Cash Flow, Claim Denials & Compliance Risk
- Reimbursement: Correct modifier use can mean full payment, and errors can cause payers to bundle services or deny claims, reducing revenue. Cash Flow: Fewer corrections and appeals mean faster payments and lower AR days.
- Claim Denials: Incorrect or missing modifiers are a frequent reason for payer denial or edit rejection.
- Audit & Compliance: Misuse of modifiers may trigger audits, refund requests, or overpayment demands from Medicare administrative contractors and commercial payers.
Modifier Errors: How Small Mistakes Lead to Big Revenue Leakage
Even a single miscoded line with modifier 59 when documentation doesn’t support “distinct procedural service” can prompt a payer to bundle services or deny part of the payment. If your group processes 10,000 lines per month and just 1% have modifier issues, that’s 100 lines at risk—and if each loses $200, that’s $20,000 monthly revenue leak.
Modifier-Related KPIs and Benchmarks for Revenue Cycle Performance
RCM leaders should track key performance indicators, such as:
- Percentage of claims with high-risk modifiers appended (> X codes)
- Denial rate due to modifier errors
- Appeal success rate for modifier issues
- Revenue recovered via modifier correction and resubmission
Common Denials Caused Due To Modifier Misuse
Most common denials stem from using modifiers that don’t meet payer criteria. These errors usually stem from rushed coding or inconsistent interpretation of payer rules.
Incorrect or missing modifiers often surface as specific denial codes. Some of the most frequent include:
- CO-4 — Invalid modifier: Triggered when the modifier isn’t appropriate for the CPT/HCPCS code or violates payer rules.
- CO-16 — Claim lacks required information: Often used when a required modifier (e.g., 25, 59, RT/LT, 26/TC) is missing.
- PR-55 — Procedure code inconsistent with modifier used: Issued when the modifier conflicts with the service billed (e.g., incorrect anesthesia or surgical modifiers).
- CO-9 — Invalid combination of modifiers: Returned when multiple modifiers on the same line item aren’t allowed together.
Modifier 59 vs X-Modifiers: When To Use What?
Modifier 59 is one of the most commonly used modifiers in medical billing, but many payers and CMS now prefer more specific alternatives such as XE, XS, XP, and XU modifiers. Using modifier 59 by default, without proper documentation, can trigger audits or claim denials.
Many billing teams still rely on it out of habit, yet payers increasingly flag its overuse as a compliance risk.
To avoid issues, coders should understand when to use modifier 59 and when an X-modifier is more appropriate. Each X-modifier—XE (separate encounter), XS (separate structure), XP (separate practitioner), and XU (unusual non-overlapping service)—offers clearer, more accurate detail, improving compliance and reimbursement outcomes.
When and Why Use Modifier 59
Modifier 59 is appropriate under certain circumstances, as noted by the CMS, such as when services occur during different sessions, at different sites or organ systems, or involve separate lesions or injuries. However, CMS guidance advises using a more specific modifier when available.
For example, if a surgeon performs an excision (CPT 11055) and a repair (CPT 12001) on the same day and site, modifier 59 may not apply unless documentation clearly supports distinct services. Reflexively appending modifier 59 without adequate documentation increases the risk of recoupment.
According to CMS guidance: Modifier 59 may be used under certain circumstances, for example, different session, different procedure, different site or organ system, separate lesion or separate injury. However, CMS guidance also notes that if an already established modifier exists that describes the circumstance more precisely, you should use that instead of 59.
Example: A surgeon performs an excision (CPT 11055) and a repair (CPT 12001) on the same day, same site. Modifier 59 may not apply if the two services are bundled; documentation must support a separate lesion or a different anatomical site.
If coders append 59 reflexively without documentation, the payer may still process, but the risk of future audit or recoupment increases.
X-Modifiers: When To Use Them?
CMS introduced the X-modifiers—XE, XS, XP, and XU—to offer greater specificity and reduce misuse of modifier 59 in medical billing. These modifiers clarify why two services performed on the same day should be paid separately instead of being bundled under National Correct Coding Initiative (NCCI) edits (CMS Distinct Procedural Services Guidance).
Each X-modifier identifies a different clinical or procedural distinction. They are designed to replace modifier 59 when more detail is available, ensuring payers receive accurate context and minimizing audit exposure. Using X-modifiers instead of modifier 59 also improves claim transparency and speeds up adjudication, especially for Medicare and commercial payers that closely monitor modifier 59 usage.
Here’s a quick reference table outlining how each X-modifier is used, along with documentation and payer guidance:
Tip: Always verify payer acceptance of X-modifiers before submission. While CMS and most major insurers accept them, a few commercial payers like Cigna and Aetna still rely on modifier 59. Use X-modifiers when documentation supports the specific distinction (separate encounter, structure, practitioner, or non-overlapping service) to strengthen compliance and reduce the chance of post-payment audits.
What Are The Documentation Requirements for Common Billing Modifiers?
Any good revenue cycle strategy includes documentation checks when modifiers are used. Here’s what you need:
- Modifier 25: Documentation must demonstrate that the evaluation and management service was significant, separately identifiable, and above and beyond the other procedure, not merely preoperative preparation.
- Modifier 59/X-modifiers: Clinical notes must clearly describe separate sessions, sites, organ systems, or lesions, differentiating the service from bundled procedures.
- Modifier 26: Documentation should distinguish the professional component (e.g., physician interpretation) from the technical component (e.g., equipment use).
If documentation is weak, payers may deny or recoup. Revenue cycle leadership must establish workflows to flag modifiers that require enhanced documentation review before claim submission.
Payer-Specific Modifier Policies
Modifier rules vary by payer. Some payers have unique policies, edit logic, and preferred modifiers:
- Some require modifier 26 to bill the professional component for imaging, while others bundle professional and technical components.
- Medicare uses modifiers GY and GZ to indicate services that are not covered or expected to be covered.
- Modifier AT is used by Medicare for chiropractic active treatment versus maintenance care.
RCM leaders must monitor each major payer’s policy for “list of modifiers in medical billing with description” and integrate that into submission workflows. Having a payer-policy library with modifier precedence and edit rules is a high-value asset.
How CombineHealth Can Help with Modifier Management
Manual review of modifier use is laborious, error-prone, and costly. That’s where automation and AI step in:
- Real-time modifier suggestion: CombineHealth’s Amy AI monitors CPT/HCPCS pairs, payer policy updates, and NCCI edits, then suggests the correct modifier (e.g., 25 vs 59 vs XS) based on documentation context and past payer behavior.
- Documentation-matching: The system flags cases where modifier 25 is appended but the note does not clearly show a “separate and identifiable E/M”.
- Claims pre-submission validation: The AI platform runs each claim through a modifier-check logic (pricing vs informational modifiers, payer-specific rules) and prevents submission if high risk of error.
- Trend analytics: Dashboards highlight which modifiers cause denials or underpayments, enabling targeted audits and staff training.
By integrating AI into your modifier workflow, you minimize incorrect modifier use, reduce denials, and recoup more revenue. The goal is fewer “modifier misuse” losses and fewer audit headaches.
Strengthen Compliance and Revenue with Smarter Modifier Management
Accurate modifier use is one of the most effective ways to protect revenue and maintain compliance in healthcare revenue cycle management. Applying the correct modifier—whether it’s modifier 25, 59, 26, or 76—reduces denials, ensures accurate reimbursement, and minimizes administrative burden.
Even small coding errors or guesswork can cause significant revenue loss and back-office strain. To stay ahead, RCM teams should:
- Build structured workflows for modifier selection and documentation.
- Maintain an up-to-date payer-specific modifier policy library.
- Track KPIs related to modifier-linked denials and appeals.
- Use AI-driven tools to verify modifiers and match documentation in real time.
Approaching modifier management as both a compliance requirement and a strategic revenue lever can transform billing accuracy and financial performance.
To see how intelligent automation can simplify modifier validation, improve coding precision, and accelerate reimbursements, schedule a demo with CombineHealth today.
FAQs
What is modifier 25 in medical billing?
Modifier 25 is appended to an E/M code when a significant, separately identifiable evaluation and management service is performed by the same physician on the same day as another procedure or service.
When should you use modifier 59 in medical billing?
Modifier 59 is used to indicate a distinct procedural service in circumstances where another code in the day is normally bundled—but only when documentation supports a separate session, site, or service and no more descriptive modifier is available.
Can AI help reduce modifier-related denials?
Yes. AI systems can validate modifier logic before submission, match documentation to required modifiers (e.g., separate E/M or distinct service), and provide analytics on which modifiers are causing denials or under-payments. This leads to fewer manual reviews and stronger revenue capture.
What is the list of modifiers in medical billing?
There are hundreds of CPT and HCPCS modifiers. Providers should refer to the AMA CPT manual, CMS HCPCS modifiers list, and payer-specific references. Common ones include 25, 26, 59, 76, XS, JW, GY, GZ, 50, and many others.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.png)
.webp)









