Building a Smarter Prior Authorization Process: Insights from a Transactional Leader at HCA Mission Health
Discover insights on building a smart prior authorization process from a seasoned RCM leader with 36 years’ experience on both payer and provider sides.
September 19, 2025

Imagine flipping through thick paper catalogs, trying to figure out which procedures required prior authorization—only to update them again the next day because a payer changed the rules.
That was Marc McCauley’s world when he first entered the revenue cycle space, only that he wasn’t the one flipping the binders, but was actually setting those rules on the payers’ side.
For nearly two decades, he worked with the top five insurance companies adjusting claims, writing contracts, and learning exactly how insurers made their decisions. Later, he crossed over to the provider side, where he built and led teams tasked with securing those same authorizations.
Now, with 36 years under his belt and as a Director of Physician Services at HCA Mission Health, Marc has seen prior authorization in healthcare evolve—from binders and fax machines to payer portals and AI. And he knows which parts of the process are timeless.
This blog captures Marc’s hard-earned lessons on how to build a smarter prior authorization process in healthcare as someone who’s played on both sides of the field.
What Is Prior Authorization in Healthcare and Why Is It Important?
Prior authorization is a process used by health insurance payers that requires providers to get advance approval from the insurer before delivering certain services, treatments, procedures, medications, or medical equipment.
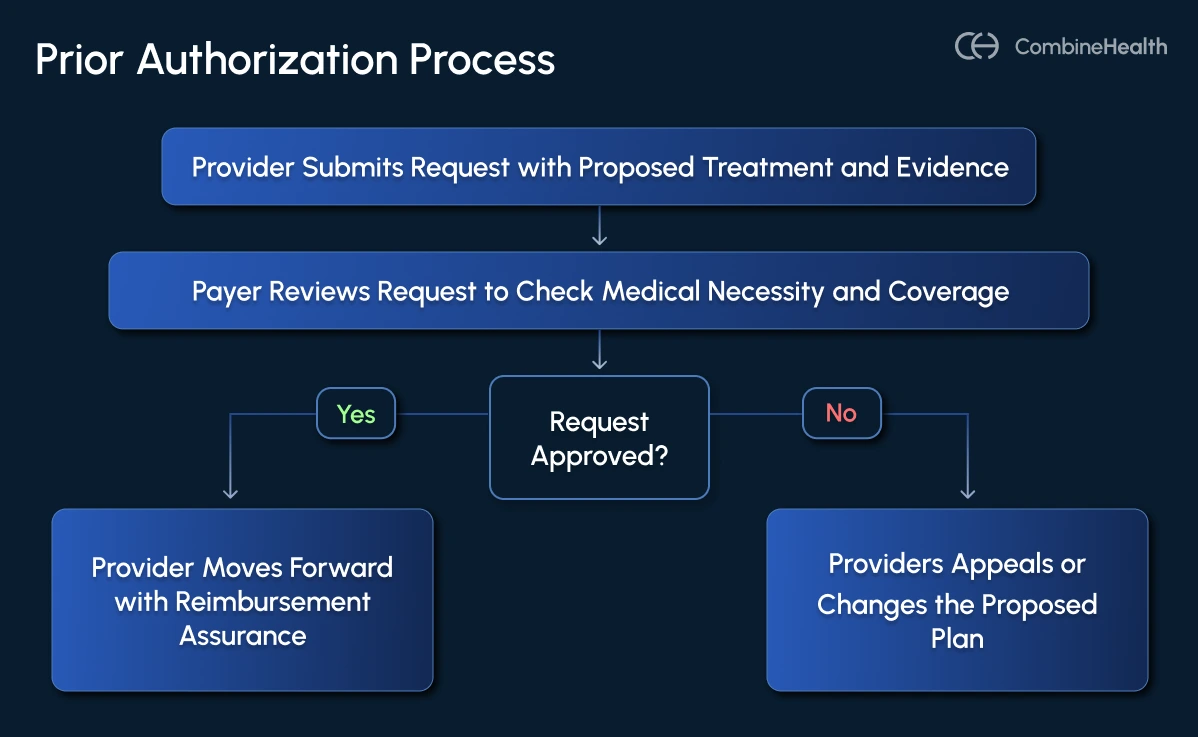
Here’s how the prior auth process typically works:
- Provider submits a request that includes patient information, diagnosis, proposed treatment, and supporting clinical evidence
- Payer reviews the request to see if the proposed service is medically necessary, cost-effective, and if it complies with their coverage rules
- If approved, the provider can move forward with the service with assurance (or a higher likelihood) of payment. If denied, it can lead to denial appeals or changes in the proposed plan
What Role Does Prior Authorization Play in the Revenue Cycle?
Prior authorization applies across the spectrum of care, from routine office visits to complex surgical procedures.
While authorizations for office visits are usually straightforward, the stakes rise significantly with high-value services, such as surgeries. These are the cases where most of a hospital’s revenue sits.
Marc noted that prior authorizations don’t always guarantee smooth sailing. Surgeons may enter the operating room expecting to perform one procedure but pivot to another once they assess the patient’s condition. If the new procedure isn’t covered under the existing authorization, the claim can be denied unless the team pivots quickly—sometimes within 24 hours.
.webp)
In other words, missing an office visit prior authorization might mean losing $100, but missing a neurosurgery prior authorization could cost an organization tens of thousands.
How To Build Your Prior Authorization Workforce
For transactional leaders in RCM, prior authorization is about building a system strong enough to withstand constant payer changes, staff turnover, and clinical curveballs. The workforce you put in place is the backbone of that system.
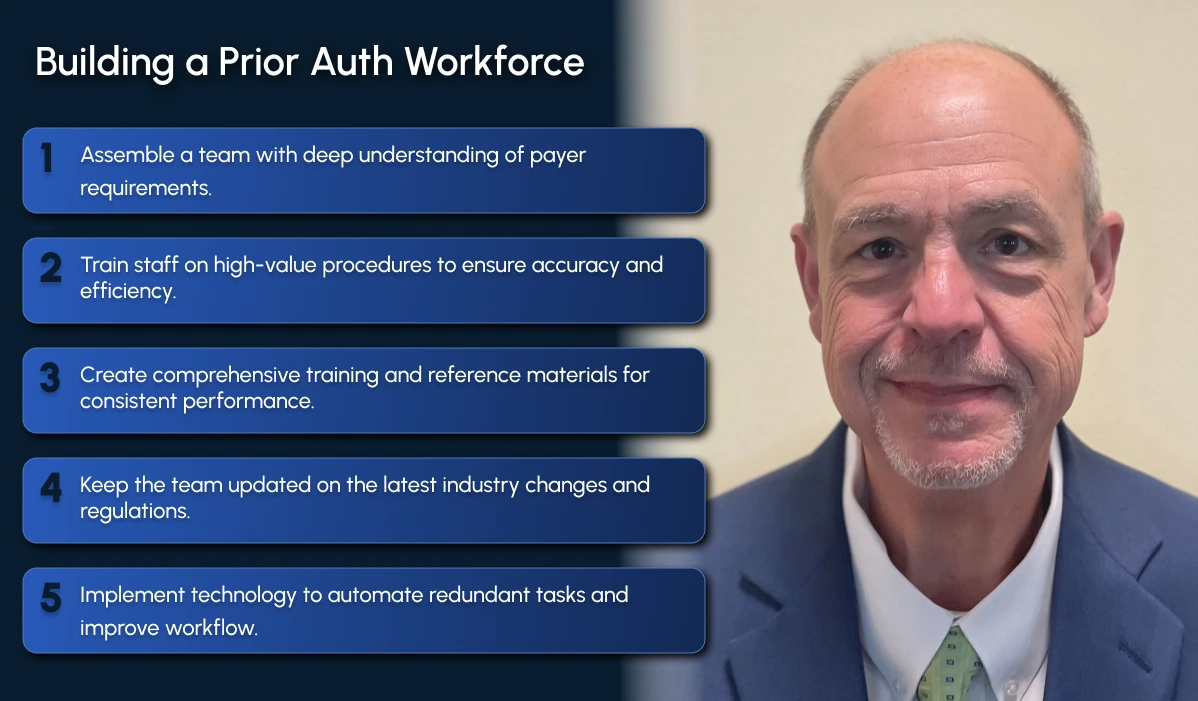
1. Build a Payer-Savvy Team
Not all payers are alike, and a one-size-fits-all approach rarely works.
A good practice is to hire specialists who know the ins and outs of particular carriers. For example, onboard one team member focusing on Blue Cross Blue Shield prior auth, another on Cigna prior auth, and the next on United Healthcare prior auth.
Over time, these staff learn the “tricks of the trade” for their assigned payer and become go-to experts for the rest of the team.
2. Coach Your Staff Around High-Value Procedures
Actively coach staff on how to approach prior authorization requests for complex procedures:
- What documentation is needed
- How to anticipate payer questions
- How to act quickly if the plan changes mid-surgery
Know exactly which procedures at your clinic or hospital require prior authorization and keep that list updated. This not only reduces guesswork but also forms the basis of your training materials.
3. Develop Training and Reference Materials
Turn process documents into training guides. When a staff member turns over (as it often happens in healthcare RCM), well-documented workflows, cheat sheets, and payer-specific quick reference guides will speed up onboarding and maintain consistency.
4. Stay Informed and Keep Your Team Informed
Sign up for payer newsletters, and encourage your staff to do the same. Policy updates are often buried in those bulletins. Beyond newsletters, professional organizations like AAPC and MGMA, along with conferences and workshops, can help leaders stay ahead of changes.
.webp)
5. Embrace Technology For Redundant, Tedious Tasks
The days of handwritten notes and binders of payer rules are gone. Use electronic documentation tools that can be shared across the team, updated in real time, and searched quickly. A central knowledge base or shared OneNote, for example, can become a team’s most valuable resource.
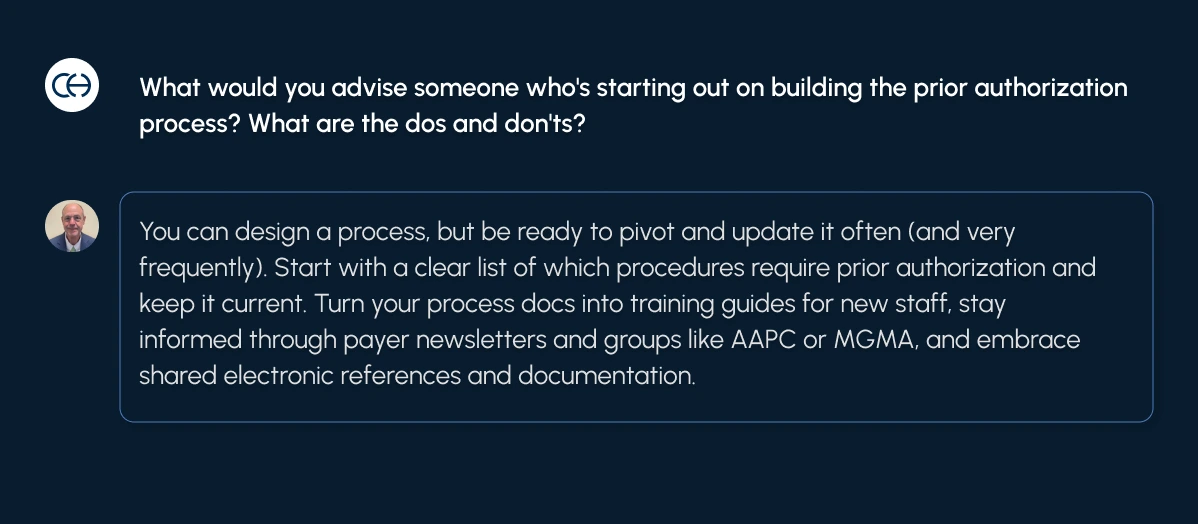
Setting Up a Robust Prior Authorization Process
A robust prior authorization process for providers involves building a system that anticipates changes, prevents costly mistakes, and creates a safety net when denials occur.
Here’s how you can do that:
1. Enforce Strong Communication Workflows
A robust prior authorization process starts with thinking through each step before a claim ever goes out the door.
As Marc explained, even the best-laid surgical plans can change mid-procedure. That’s why active communication between the provider in the OR and the prior authorization staff is essential.
2. Maintain Clear Clinical Documentation
Marc stressed that every conversation with an insurance company should be recorded and well-documented. This includes keeping a record of:
- Who you spoke to
- What was said
- When you appealed (and how many times)
.webp)
How To Effectively Track Prior Authorization Related Denials
Marc emphasized that denial management isn’t about reacting blindly—it’s about tracking, trending, and analyzing denials in detail.
Get to the Root Cause
The first thing Marc advises when it comes to managing denials is to question every prior authorization denial you get. Never believe it to be true unless you’ve found the root cause of it.
A lot of procedures don’t even require prior authorization (like on Medicare). But if you still see a prior authorization-related denial for that payer, this means the insurance company is at fault.
Sometimes it could be a network denial where the provider wasn’t listed as in-network. This happens a lot because insurance companies don’t regularly update their provider networks.
If the team treats all these denials as the same, they’ll apply the wrong fix and waste valuable time. Marc called root cause analysis the number one skill in revenue cycle management, because only by uncovering the true reason for a denial can teams prevent it from happening again.
Break Down Denials by Carrier
Not all payers behave the same way, and lumping all prior authorization denials together hides important details.
One carrier might deny claims because its network files are outdated, while another may be stricter about clinical documentation. Marc advised leaders to separate denials by payer so that recurring issues can be spotted and fixed at the source.
Separate by Type of Service
Denials don’t just differ by payer; they also vary by the type of service. Office visit (E/M) denials are often straightforward, but surgical procedure denials can be far more complex and costly.
By categorizing denials into service types, RCM teams can prioritize the high-value ones and focus their efforts where the financial stakes are highest.
Use Technology to Spot Denial Trends
Most EMRs can export denial data, but raw lists aren’t enough. Marc suggested building pivot tables or reports to organize this data into clear trends.
With the right use of spreadsheets or analytics tools, patterns emerge—like a spike in denials for one procedure code or a specific payer. This turns denial management from a reactive process into a proactive strategy.
Recommended read: An expert-backed playbook on denial management
Involving Patients in the Prior Authorization Process
Many patients assume that prior authorizations are handled entirely by the provider’s office, but their involvement matters just as much.
When an authorization is denied, teams often need to involve the patient directly—giving them the insurer’s contact information and encouraging them to advocate on their own behalf.
That said, transparency about the whole process is equally important. Keeping families informed about delays or denials can turn them into valuable allies, rather than leaving them frustrated.
In Marc’s experience, patients are often willing to step in and push their insurers if they understand what’s at stake.
Educating Patients on Prior Authorization: Best Practices
For surgical cases, proactive education works best. That’s because in such cases, patients could use a clear, simple overview of what the prior authorization process for providers will look like before they can move forward with treatment.
A good approach is to give them a visual guide that outlines:
- The steps involved
- Expected timelines
- Common payer requirements
Marc backed this up by sharing an interesting anecdote:
“When I was managing a neurosurgical team in Florida, we explained the prior auth process to patients in a pictorial way. So, when we had patients coming in for surgery, the scheduler could walk them through a simple visual guide showing each step—from the doctor’s visit to the prior auth checks.
We even included timelines (30, 60, or 90 days) and highlighted requirements insurers often imposed, like six months of physical therapy or smoking cessation.”
Without this context, many patients assume that surgery can be scheduled right away, only to be surprised by long delays. And when payers refuse to budge, patients can even escalate the matter to the state insurance commissioner, who has the authority to hold carriers accountable.
.webp)
How Has Technology Evolved in the Prior Authorization Space Over Time
Marc has seen prior authorization workflows transform dramatically over the past three decades.
Early in his career, the process was entirely manual. Teams kept payer requirements in paper catalogs—literally flipping through binders to check if Blue Cross or Aetna required authorization for a given procedure. These catalogs had to be updated constantly, often daily, as payer rules changed.
The next phase brought phones and fax machines. Staff spent hours calling insurers for approvals or sending documents via fax. While this reduced the reliance on paper catalogs, it still consumed enormous amounts of time and left room for errors.
Today, most prior authorizations are submitted online through payer portals or automated software that integrates with EMRs. Some platforms can pre-populate request forms with patient demographics, diagnosis, and order details, and even track the status in real time. This has drastically cut down the manual back-and-forth, though payer variability still creates friction.
AI & the Future of Prior Authorization
Looking ahead, Marc predicts that AI will reshape the space further. He believes both insurers and providers are racing to use AI to outpace one another.
On the payer side, AI is already being used to scan claims and analyze medical records. For providers, the opportunity lies in turning denial data and payer newsletters into machine-readable formats to build algorithms that anticipate payer behavior.
Marc described this moment as a competition—both sides racing to outpace one another with AI tools.
Recommended read: Tough questions to ask while evaluating an RCM coding and billing software
Marc’s Advice to Budding RCM Leaders
Marc’s message to new RCM leaders is simple: know the work yourself before you can lead others through it.
To train and coach effectively, you have to understand:
- What your staff should be doing
- How payers operate
- Where mistakes happen
He also advised leaders to monitor staff productivity closely. That includes watching how far out authorizations are being obtained—at least two weeks ahead for office visits, and often months ahead for surgical procedures.
That’s because data and metrics only tell part of the story; the rest comes from being close enough to the process to spot problems in real time.
Curious to know how CombineHealth AI agents can help with prior authorization? Book a demo!
FAQs
What is the prior authorization process?
Prior authorization is when a healthcare provider must get approval from an insurance company before delivering certain services, procedures, or medications to ensure coverage.
How long does the prior authorization process typically take?
The prior auth process can take a few days to several weeks, depending on the payer and service. Simple authorizations move faster than complex surgical ones.
Who typically initiates the prior authorization process?
The provider’s office or care team usually initiates the request, submitting required documentation to the insurance company on the patient’s behalf.
How does the prior authorization process work?
The provider submits clinical and administrative details to the insurer, who reviews them against coverage rules. Approval allows the service to proceed; denial may require an appeal.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















