2025 Buyer’s Guide for CDI Software: Key Features, KPIs, and Selection Tips
Can't make up your mind on which CDI software to invest in? Check out our comprehensive guide to understand the features to look for and the KPIs to track to find the perfect match for your CDI efforts.
July 30, 2025


Key Takeaways
• Traditional CDI processes are labor-intensive, retrospective, and often too late to prevent documentation errors or claim denials.
• Fragmented tools, rising volume, or limited staff are signs that it’s time for CDI automation.
• CDI tools that explain coding logic clearly, integrate into your EHR, and support real-time query resolution make adoption smoother.
• Generic CDI tools fall short in complex specialties like orthopedics and cardiology. Look for solutions that handle documentation, coding, and claim creation, all in one place.
• Measure the CDI impact with actionable metrics like query resolution rates, DRG shifts, cash acceleration, and provider turnaround time
If you’re managing documentation and coding for a busy practice or hospital, you’ve probably thought about investing in CDI software.
But choosing one? That’s a lot harder.
And there’s no shortage of advice out there on selecting a CDI software, focused on streamlining documentation, reducing denials, and improving accuracy.
The truth is, finding the right CDI tool isn't just about checking off features on a comparison chart. It’s about understanding your team’s real challenges, like:
- Coders waiting on documentation that’s missing key details
- Providers burning out from back-and-forth queries
- Billing teams stuck cleaning up gaps after claims have gone out
That’s why we’ve shaped this guide with conversations we’ve had with experts (RCM leaders, practice managers, clinicians), talking openly about the gaps they’ve run into, and what finally made them start looking for help.
Drawbacks of A Manual CDI Program
Let’s start by revisiting what traditional CDI programs looked like and why they no longer scale for most teams today.
The traditional CDI program involved a team of CDI specialists, often nurses with medical coding backgrounds or medical coders with CDI training, to review clinical documentation.
The review would happen occasionally, where a handful of cases are randomly picked and assessed for issues like:
- Nonspecific terminology
- Uncertain diagnoses
- Unaddressed diagnostic test results
- Missing information from diagnostic findings and treatment processes
.webp)
Typically, the process involved a back-and-forth between CDI specialists, medical coders, and providers. Here’s what it looked like:
- When CDI specialists spotted documentation gaps, they would send a clarification query to the provider.
- Specialists had to track responses manually, send reminders, and often wait days for resolution. It was a high-touch, low-scale process.
- Clinicians would take out additional time from their shifts to address the queries and fix documentation issues for future encounters.
The setback of the traditional approach?
These reviews typically happened after the encounter, when care decisions had already been made and claims submitted. It was too late to fix errors in real time.
Also, without structured systems, hospitals struggled to measure the true impact of CDI. Data was tracked manually, and performance metrics were inconsistent.
When Do You Need CDI Software?
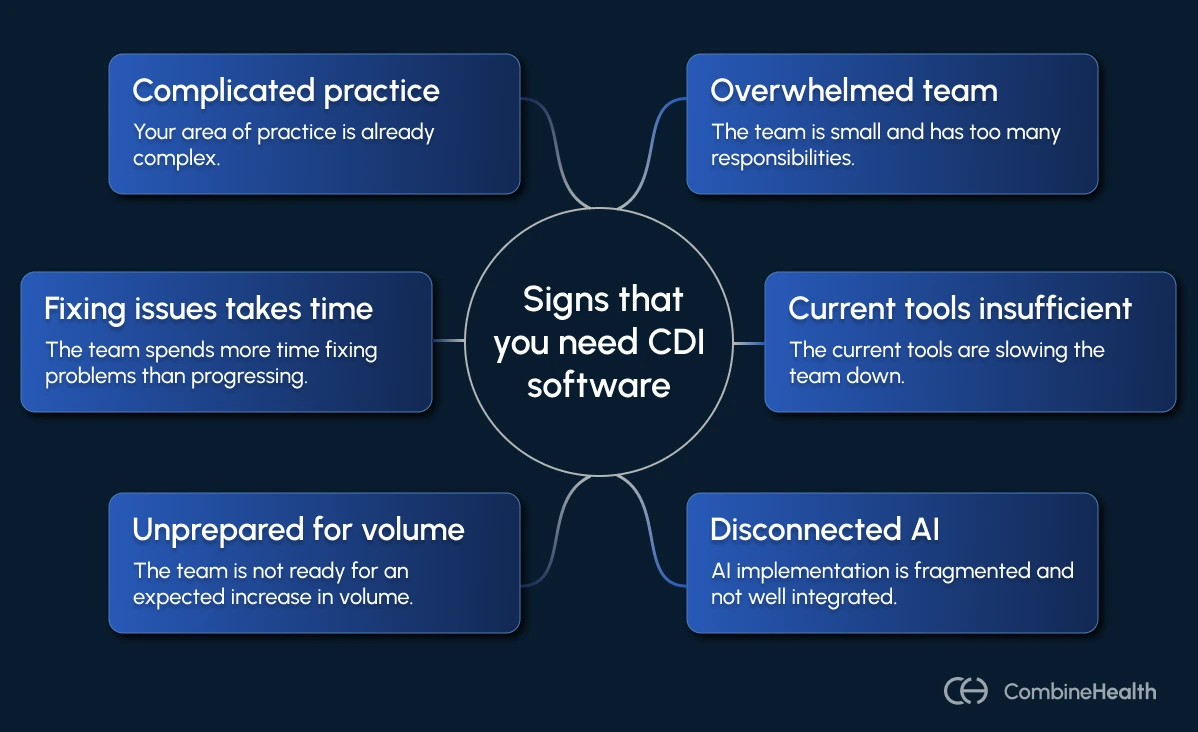
Based on what our prospects and customers have shared with us, here are the most common signs it's time to bring in technology that can actually help:
1. You’re A Small Team Wearing Too Many Hats
One of our customers runs a small surgical practice where he single-handedly takes care of the entire revenue cycle. He’s handling coding, submitting claims, managing denials, and even writing appeals—all without a certified coder on staff.
“If AI can take over those smaller tasks so we can put more attention to the patients, we’re all about that. Right now, we’re just getting by.”
As a result, when that one person goes on a break, the entire process slows down.
When clinical and billing teams are lean, there's no room for manual workarounds. And CDI software helps multiply your output, without multiplying your headcount.
2. Your Current CDI Tools Are Dragging You Down
Some teams spend hours inside systems that aren’t built for scale. Whether it's a laggy EHR or a clunky coding interface, the issue is the same: some systems weren’t built for scale, transparency, or the realities of modern healthcare documentation.
Most of our customers who first approached us to switch from another RCM tool to CombineHealth had one concern: “I didn’t understand the product. I didn’t know where to go to fix things.”
Even when documentation exists, it’s often scattered—progress notes in one tab, labs in another, handwritten notes in a file, coding queues somewhere else. That fragmentation slows everything down: reviews, coding, claim creation, and appeals.
3. You’ve Tried AI in Pieces—But Nothing’s Really Connected
When asked one of our customers about their use of AI tools in their CDI process, they said:
“We use it a little bit… there’s nothing official. I’m just trying to make it fit in different pieces.”
Like them, a lot of healthcare organizations are experimenting with AI. Some providers dabble in ChatGPT for coding tips or appeal drafting, while some use AI scribing tools to ease their documentation tasks.
But since most of the work is fragmented, nothing ever touches the actual CDI workflow.
The result? No standardized process, no audit trail, and no meaningful reduction in documentation gaps or denials. You’re still flying blind and still relying on manual reviews to catch what AI missed.
What you need is one system that ties everything together—where AI helps from documentation through to denial resolution.
4. You Expect A Surge in Volume—But You’re Not Ready
A coding manager for an anaesthesia specialty services company was managing 30 claims a day manually, which seemed doable at first. But, as they expanded contracts with major hospital systems and started accepting more insurance types, they knew the volume was about to explode.
The problem? Their documentation and coding workflows weren’t built for scale. They had one coder and one denial manager handling manual submissions and retrospective chart views.
A CDI software that surfaces gaps in real-time (not after the fact) and standardizes documentation is what you need to fix this problem.
5. Your Team Spends More Time Fixing than Moving Forward
If your staff spends the day fixing claim errors, manually applying payments, or chasing incomplete documentation, you’re in reactive mode.
One of our customers put it bluntly:
“I was fixing $278 on one claim and don’t even know why. The system didn’t apply it right, and I was just trying to constantly correct things that should’ve been done right the first time.”
Sounds familiar?
This customer wasn’t short on skill. What they lacked was a system that could catch problems before they became denials.
6. Your Specialty of Practice is Complicated Enough
Some specialties are just inherently complex. Think cardiology, orthopedics, emergency medicine, psychiatry, and departments where:
- Patients present with overlapping conditions
- Clinical decisions rely heavily on test interpretations
- Treatments often involve multi-stage plans or coordination across specialties
And in these scenarios, CDI becomes especially critical since vague documentation can downcode an encounter or delay treatment.
Factors To Consider When Purchasing a CDI Software
Choosing the right CDI software is about finding a system that supports your workflows, integrates cleanly, and genuinely helps your teams do better work with less burnout.
Based on what we’ve learnt from real pain points of our prospects and customers, here are some factors to consider when making the choice:
Buy-In From Coders, Providers, and CDI Specialists
No CDI software works unless the people using it want to use it.
When evaluating a tool, consider these questions:
- Will providers feel like it actually helps them document faster and more accurately?
- Will coders understand the logic behind the suggested codes or feel like they’re working against a black box?
- Can CDI specialists collaborate without friction?
In short, no matter how good a CDI software is, if the adoption is poor, it’s probably not worth your investment.
In our experience, the tools that earn real trust across teams do a few things exceptionally well:
- They have clean interfaces and dashboards that allow users to see every useful metric clearly
- They provide coders with clear, rational explanations for every code and modifier
Integration With Your EHR
Many healthcare organizations have clinical documentation happening in one system, coding in another, billing in a third, and queries are managed somewhere in a spreadsheet or email inbox.
Such disjointed systems create real pain for teams:
- Providers have to copy-paste notes from one tab to another.
- Coders often have to wait for documentation to be finalized, signed, or manually exported before they can even begin their work.
- CDI teams flag issues that get buried in a different system entirely
Before you commit to any CDI software, ask these questions:
- Can it pull in real-time data from your EHR, including both structured fields and narrative notes?
- Can it write back completed encounter notes or coding decisions without requiring another system login?
- Does it reduce the number of clicks it takes for a provider to finish documentation or add to it?
Analytics Dashboard to Help You Measure the Impact of Your CDI Program
In six months, if someone asks you, “Is this CDI program actually working?” and you’re still not quite sure, your current process might be lacking the crucial insights.
We’ve seen this play out in organizations of every size:
Great CDI programs quietly do important work, but with no way to show their impact clearly. No data to defend staffing needs. No visibility into whether documentation improvements are reducing audit risk or lifting the case mix index.
When evaluating CDI software, don’t just ask if it comes with “reporting.” Ask:
- Can you track query volumes, provider response time, and documentation improvement trends over time?
- Can you segment performance by location, specialty, or provider?
- Does the dashboard show pre- vs post-intervention outcomes, like changes in severity scoring, DRG assignments, or denial rates?
Customer Support That Feels Like a Partner
You don’t realize how important support is until you really need it.
Maybe a provider is struggling to finish a note.
Maybe a coder flags something odd in how documentation is being interpreted.
Maybe you just need to customize the way your team handles queries, and you’re not sure where to start.
In moments like these, you don’t want to submit a ticket and wait 72 hours just to get a generic answer. You want support from someone who understands clinical workflows, revenue cycle pressure, and how small technical issues can snowball into operational delays.
Customer Reviews That Reflect Real RCM Pain Points
When you're shopping for CDI software, the reviews matter, but only if they're coming from the right people.
Generic five-star ratings or an award from some market research company won’t tell you much. Vendors most often pay money to get those. What you need is to hear from folks who’ve had specific use cases where an AI CDI tool helped them solve a problem.
When researching a product, look at their case studies and the results they were able to drive for their customers. See if you resonate with the problem they solved. If their customers sound like your team and they’re still happy months later, you might be looking at the right solution.
Also, don’t forget to explore independent marketplaces like Elion, which feature verified healthcare technology vendors. Marketplaces like these often offer peer-reviewed evaluations, product comparisons, and customer insights that go beyond polished marketing pages.
Support for Specialty Practices
The way a family medicine provider documents a routine visit is entirely different from how an orthopedic surgeon, psychiatry, or behavioral health specialist documents a complex case. Yet, too many CDI tools treat every specialty the same with rigid templates, generic alerts, and cookie-cutter logic.
When evaluating a CDI tool, ask these questions:
- Can it handle specialty-specific documentation and coding nuances?
- Does it flag missing clinical indicators relevant to your field—not just general best practices?
- Can it detect unsupported or ambiguous diagnoses in real time?
RCM Coverage
CDI is only a step in the revenue cycle management process. And each step in the RCM process plays a role in whether your organization gets reimbursed properly.
That’s why you should think beyond documentation when evaluating CDI software. Ask:
- Does it help you generate clean claims automatically from encounter notes?
- Does it surface payer-specific rules, bundling requirements, or modifier issues early?
- Can it flag denials as they happen and suggest possible fixes or clarifications?
- Does it support eligibility verification, coding audits, or appeal support?
KPIs of A CDI Software: How To Measure Your CDI Success
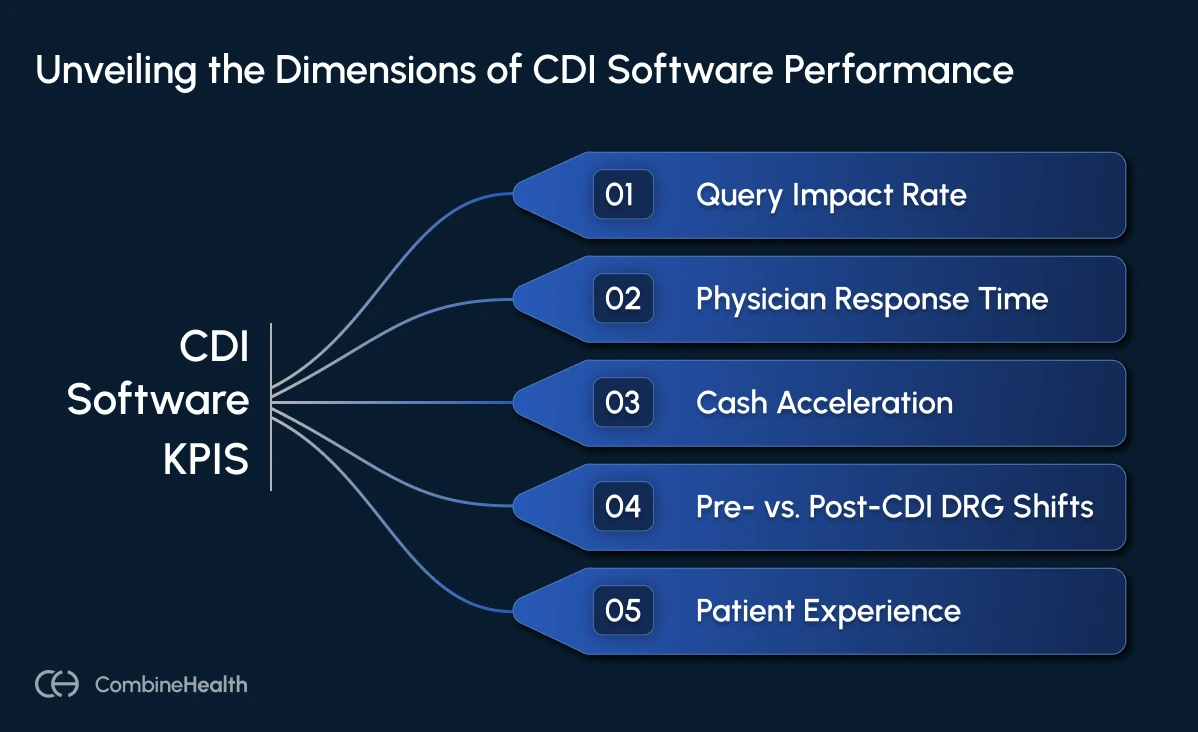
Once your CDI software is live, the big question becomes: Is it actually helping?
The answer lies in the data that shows how documentation improvement is affecting reimbursement, clinical clarity, and even patient care.
Here are the top five CDI metrics that matter the most:
1. Query Impact Rate
A high query count doesn't mean your program is effective. It just means your reviewers are busy. What matters is whether those queries actually change outcomes.
To measure the impact of the queries, track these metrics:
- Number of queries that resulted in a diagnosis change
- Number of queries that lead to a DRG shift
- Financial impact per resolved query
- Query types with the highest downstream impact (e.g., MCC capture, specificity clarification)
2. Provider Response Time
If your CDI software integrates well with provider workflows, you’ll notice less resistance and quicker resolution. Track these metrics:
- Average time to respond to queries
- Percentage of queries resolved within 24–48 hours
- Provider satisfaction or compliance with query requests
3. Cash Acceleration
One of the most concrete outcomes of strong CDI? Faster payments.
When documentation is complete and accurate upfront, claims move faster through coding, billing, and reimbursement. To measure the impact on cash acceleration, track these metrics:
- Days in accounts receivable (AR)
- Time from patient encounter to payment received
- Percentage of claims processed on first pass
4. Pre- vs. Post-CDI DRG Shifts
A pattern of appropriate DRG shifts reflects better specificity, more defensible records, and a clearer clinical picture. Track these metrics:
- The frequency of DRG changes after CDI review
- Case Mix Index (CMI) changes over time
- SOI and ROM scoring improvements
5. Patient Experience
CDI is often thought of as a financial function, but it also plays a quiet, powerful role in clinical care.
When documentation tells the full story and supports faster, better-informed decisions, it also prevents errors like:
- Missed diagnoses
- Duplicate testing
- Readmissions due to vague discharge notes
Look for metrics like readmission rates, patient complaints, and treatment delays tied to CDI issues to understand the impact of your CDI program.
Ready To Strengthen Your CDI Program With AI?
CombineHealth’s AI agents act as always-on teammates, reviewing documentation in real time, flagging gaps, and applying coding rules with precision. From scribing to coding to querying, they streamline every step of the CDI workflow so your team can focus on what matters most: delivering care and getting paid accurately.
Book a demo to see how Lia and Amy can fit into your workflow.
FAQs
What is the best way to measure the success of a CDI program?
Measure CDI success through metrics like query impact rate, provider response time, DRG shifts, and days in A/R.
Look for improved documentation quality, faster reimbursements, and fewer denials. These are signs your CDI program is driving both clinical accuracy and financial impact.
What is the most important outcome of a CDI program?
The most important outcome is accurate and complete documentation that reflects the true complexity of a patient’s condition. This leads to better coding, appropriate reimbursement, and reduced risk of audits.
What challenges exist with CDI?
Manual reviews, delayed documentation, provider resistance, and lack of visibility across teams often slow down CDI efforts and reduce their impact.
How to implement CDI?
Start with clear goals, get buy-in from providers and coders, choose software that integrates with your EHR, and track KPIs like query impact and DRG shifts.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)









