Understanding Medical Billing and How AI Can Help Augment The Process
Understand what medical billing is, how it works, and what the key challenges RCM teams are facing today. Also, explore how AI can help streamline the medical billing workflows and reduce denials.
January 13, 2026


Key Takeaways
• Medical billing is the critical process of submitting claims to insurance companies and following up until providers receive full payment for healthcare services rendered.
• The billing process involves eight essential steps, from patient registration through final payment collection, with each stage requiring accuracy to prevent costly denials and delays.
• Understanding key terminology—like superbills, clearinghouses, EOBs, ERAs, modifiers, and DRGs—is fundamental to navigating the medical billing landscape effectively.
• RCM teams face mounting challenges, including claim denial rates of 5-10%, regulatory complexity with 140,000+ annual code updates, staffing shortages, and increasing patient payment responsibility.
• AI-powered solutions can reduce denials by 20-40%, accelerate claim processing from minutes to seconds, and save an average of $118 per claim by catching errors before submission.
Medical billing represents one of the healthcare’s most critical yet complex administrative functions. With the value of private health insurance spending totaling $1.5 trillion dollars, and regulations becoming increasingly intricate, understanding the billing process has never been more important for providers, administrators, and patients alike.
This comprehensive guide explores what medical billing entails, breaks down its essential components, and examines how artificial intelligence is transforming this vital healthcare function.
What Is Medical Billing and How Does It Work?
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. It serves as the bridge between healthcare delivery and reimbursement, ensuring that doctors, hospitals, and other medical facilities receive compensation for the care they provide.
The medical billing process begins when a patient receives healthcare services and continues until the provider receives full payment for those services. This involves:
- Translating medical procedures, diagnoses, and services into standardized codes
- Submitting claims (or bills) to insurance companies or government payers
- Managing any issues that arise during payment processing.
Medical billing professionals work behind the scenes to ensure accurate claim submission, resolve payment discrepancies, and maintain the financial health of medical practices. Their work directly impacts a healthcare facility's revenue cycle and ultimately determines how quickly and completely providers are paid for their services.
What's the Difference Between Medical Coding and Medical Billing?
Medical coding translates clinical documentation into standardized diagnosis and procedure codes, while medical billing uses those codes to submit claims, follow up with payers, and collect payment.
Medical coding happens first. When you visit the doctor, and they write notes about what's wrong and what they did to help you, a medical coder reads those notes and translates them into special codes. They use code systems like:
- ICD-10 (for what's wrong with you)
- CPT (for what procedures the doctor did)
- HCPCS (for medical supplies and equipment).
Think of coders as translators who speak both "doctor language" and "insurance language."
Medical billing comes next. Once the coder assigns all the right codes, the medical biller takes those codes and creates a claim—basically a detailed invoice that gets sent to your insurance company. Then, billers make sure everything on that claim is correct and complete before sending it off. They:
- Track the claim
- Follow up if there are problems
- Handle any denials
- Work to get payment from both the insurance company and the patient
Different Terminologies/Components of Medical Billing
Medical billing comes with its own specialized vocabulary and documentation requirements. While the terminology might seem complex at first, understanding these key components is essential to grasping how the billing process works. Let's explore the most important terms and documents that form the foundation of medical billing operations:
What is a Superbill
A superbill is a detailed document that itemizes all services provided during a patient encounter. It contains essential information, including patient demographics, provider details, diagnosis codes, procedure codes, charges for each service, and any relevant modifiers. The superbill serves as the primary source document from which insurance claims are created.
Healthcare providers or their staff complete superbills after each patient visit, whether in a doctor's office, clinic, or hospital setting. This document ensures that all billable services are captured and properly documented before claims submission. For self-pay patients or those using out-of-network providers, superbills can also be given directly to patients who then submit them to their insurance companies for reimbursement.
What is a Clearinghouse
A clearinghouse in medical billing acts as an intermediary between healthcare providers and insurance payers. These organizations receive claims from providers, scrub them for errors, format them according to payer specifications, and electronically transmit them to the appropriate insurance companies.
Clearinghouses add significant value by checking claims for completeness and compliance before submission, which dramatically reduces rejection rates. They also consolidate the claims process by allowing providers to submit to multiple payers through a single portal rather than managing separate connections with each insurance company. After payers process claims, clearinghouses return remittance information back to providers, creating a seamless two-way communication channel that streamlines the entire billing cycle.
What is an Entity Code
An entity code in medical billing is a two-character alphanumeric identifier used in electronic transactions to specify what type of entity is being referenced. These codes appear in various segments of electronic claims and help payers understand the relationship between different parties involved in the billing process.
Common entity codes include IL for insured or subscriber, QC for patient when different from the subscriber, 82 for rendering provider, and 85 for billing provider. Entity codes ensure that everyone involved in a claim—from the patient to the various providers and facilities—is properly identified and categorized. This standardization prevents confusion and helps payers process claims accurately by understanding exactly who provided services, who received them, and who should be paid.
What is a TPI Number
A TPI number, or Taxpayer Identification Number, is a unique identifier assigned to healthcare providers for billing and tax purposes. In medical billing contexts, the TPI number typically refers to either an Employer Identification Number (EIN) for organizations or a Social Security Number (SSN) for individual practitioners, though individual providers often use an EIN for privacy reasons.
Insurance companies require TPI numbers on claims to properly identify the billing entity and issue payment to the correct provider or organization. This number is essential for establishing provider contracts with payers, enrolling in insurance networks, and maintaining compliance with federal regulations. The TPI number also connects to important reporting requirements for taxes and healthcare analytics, making it a critical identifier throughout the revenue cycle.
What are EOBs and ERAs
An Explanation of Benefits (EOB) is a statement sent by insurance companies to patients after a claim has been processed. It details what services were billed, how much the insurance company paid, what amount applies to deductibles or copayments, and what the patient owes. The EOB is not a bill but rather an explanation of how insurance benefits were applied to the claim.
An Electronic Remittance Advice (ERA) is the provider-facing equivalent of an EOB, delivered in electronic format directly to the healthcare provider or their billing system. ERAs contain detailed payment information, including which claims were paid, adjusted, or denied, along with reason codes explaining any adjustments or denials.
What is DRG
Diagnosis-Related Group (DRG) is a classification system used primarily in hospital billing to categorize inpatient stays into groups based on diagnosis, procedures performed, age, sex, and complications. Each DRG has a predetermined payment amount that Medicare and many other insurers will pay for that category of hospital stay, regardless of the actual costs incurred.
The DRG system was designed to incentivize efficiency by paying a fixed amount per case rather than reimbursing for each individual service. Hospitals that can provide quality care while keeping costs below the DRG payment earn a profit, while those with costs exceeding the DRG payment absorb the loss.
What are Modifiers
Modifiers are two-character codes (either two digits or a letter followed by a digit) appended to procedure codes to provide additional information about the service performed. They indicate that a service or procedure has been altered in some way without changing its basic definition, such as being performed on a specific body part, by a particular provider type, or under unusual circumstances.
Common modifiers include 25, which indicates a separately identifiable evaluation and management service on the same day as a procedure; 59, which identifies a distinct procedural service; and LT or RT, which specify left or right sides of the body.
Proper modifier usage is essential for accurate reimbursement and avoiding claim denials. Using the wrong modifier or failing to use a required one can result in reduced payment, claim rejection, or even allegations of improper billing.
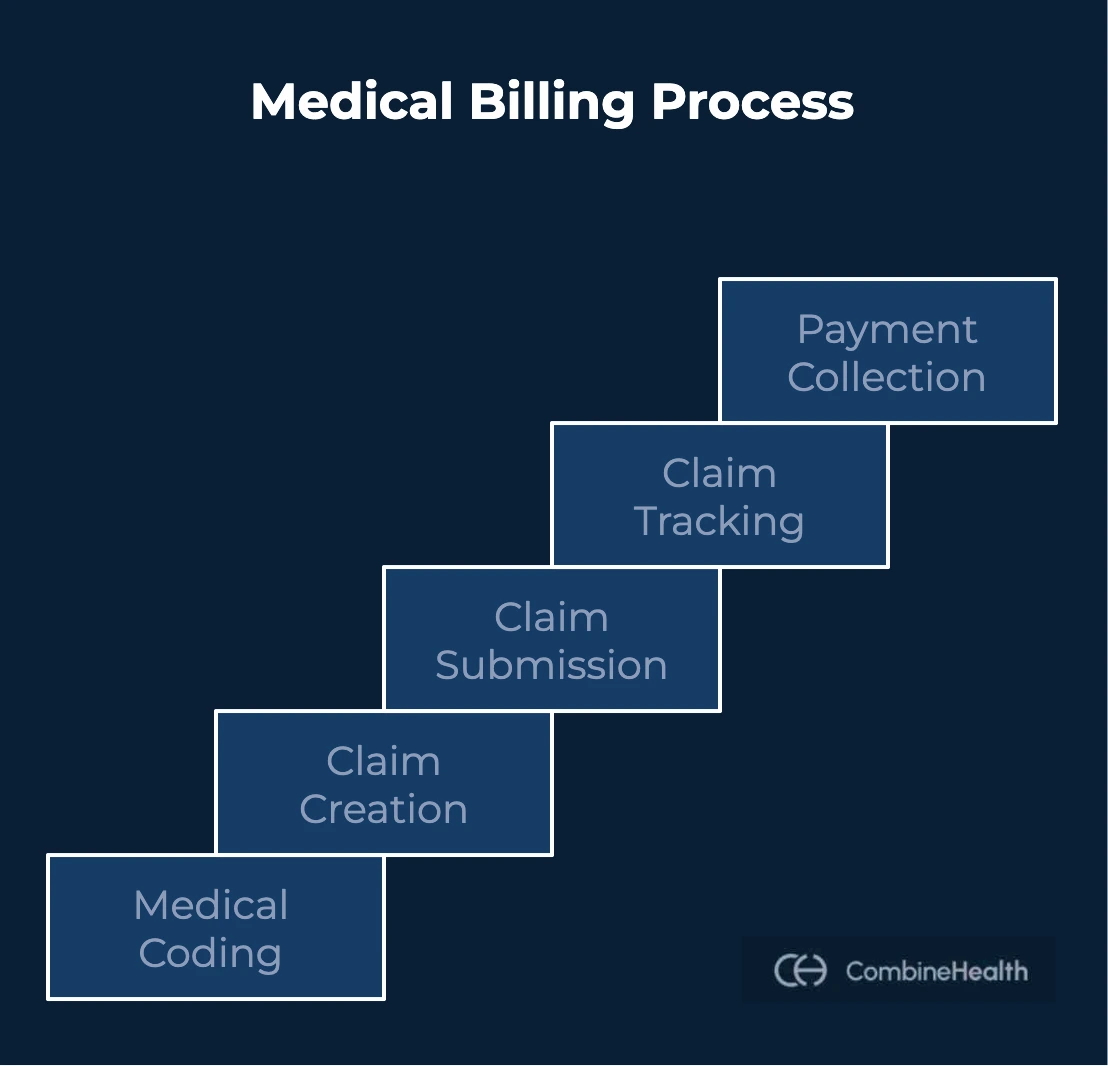
The Complete Medical Billing Process
Medical billing follows a systematic process that begins when a patient schedules an appointment and continues through final payment collection. Each step builds on the previous one, and it is important to understand the nuances of each step since errors at any stage can disrupt the entire revenue cycle.
Step 1: Patient Registration
The medical billing process begins with patient registration, which occurs before any services are provided. During registration, the practice collects demographic information, including:
- Patient's name
- Date of birth
- Address
- Contact information
- Emergency contacts
Equally important is gathering insurance information, including the insurance company name, policy number, group number, and the name of the primary policyholder if different from the patient.
Registration staff verify that all information is accurate and complete, as errors at this stage often lead to claim denials later.
Many practices now ask patients to arrive early or complete registration forms online before their appointments to ensure this critical step receives adequate attention. In some cases, front desk personnel also collect copies of insurance cards and photo identification, which help verify patient identity and insurance coverage.
Step 2: Determining Financial Responsibility
After registration, staff must determine financial responsibility by verifying the patient's insurance coverage and benefits. This process is called insurance verification or eligibility checking, and it involves verifying the following patient details:
- Patient's insurance status (active/inactive)
- Services covered under the plan
- Cost-sharing requirements like copayments, coinsurance, and deductibles
Verification also reveals important details such as whether prior authorization is required for planned services, what the patient's remaining deductible amount is, and whether there are any limitations on coverage for specific procedures.
Many practices verify insurance in real-time before appointments to avoid surprises and collect patient responsibility amounts upfront.
Step 3: Capturing Codes
During or immediately after the patient encounter, clinical staff document all services provided, diagnoses identified, and procedures performed.
Medical coders then review this documentation and assign appropriate diagnosis codes using the ICD-10 system and procedure codes using CPT and HCPCS code sets. This translation from clinical language to standardized codes is critical, as these codes determine what will be billed and how much will be reimbursed.
Accurate code capture requires detailed clinical documentation that supports the codes assigned. Coders must understand medical terminology, anatomy, and disease processes, as well as the complex coding guidelines that govern code selection. They also must ensure that diagnosis codes support the medical necessity of procedures performed, as payers will deny claims for services not deemed medically necessary.
.webp)
Step 4: Creating the Superbill
Once codes are assigned, the billing staff creates a superbill that compiles all the information needed to submit a claim. This includes:
- Patient demographics
- Insurance information
- Provider details
- Service dates
- Procedure codes
- Diagnosis codes
- Charges
- Any necessary modifiers
This comprehensive record ensures that nothing is overlooked when creating the actual insurance claim.
In many modern practices, superbill creation is automated through electronic health record (EHR) or practice management systems that pull information directly from the encounter documentation. However, billing staff still review superbills for accuracy and completeness before proceeding to claim generation. They verify that all required information is present, codes are appropriate and supported, and charges match the facility's fee schedule.
Step 5: Preparing and Submitting Claims
With the superbill completed, billing specialists create and submit claims to the appropriate insurance payers. Most claims today are submitted electronically through clearinghouses, which format the data according to HIPAA standards and payer-specific requirements. The claim includes all information from the superbill, along with additional required data elements such as provider NPI numbers, place of service codes, and tax identification numbers.
Before submission, many practices perform internal claim scrubbing using specialized AI solutions that check for common errors, missing information, and compliance issues. This quality control step catches problems before claims reach payers, dramatically reducing rejection rates.
Once scrubbed and validated, claims are transmitted to the clearinghouse, which performs additional edits before forwarding to payers. The practice receives confirmation of claim submission and can track the claim's status as it moves through the payer's system. Timely claim submission is essential, as most payers have strict filing deadlines beyond which they will not accept claims.
Step 6: Monitoring Payer Adjudication
After claim submission, the insurance company processes the claim through a series of automated and manual reviews called adjudication. During this stage, the payer:
- Verifies patient eligibility
- Confirms coverage for the services billed
- Checks for medical necessity
- Reviews coding accuracy
- Calculates payment based on contracted rates and patient benefits
This process can take anywhere from a few days to several weeks, depending on the payer and claim complexity.
Billing staff actively monitors submitted claims to ensure they are being processed and to quickly identify any that are rejected or denied. Modern AI solutions provide dashboards showing analysis of claim status and aging, allowing billers to prioritize follow-up efforts.
If a claim is denied, staff review the denial reason codes provided by the payer and determine whether the claim can be corrected and resubmitted or if an appeal is warranted.
Step 7: Creating Patient Statements
After the insurance company processes the claim and pays their portion, any remaining balance becomes the patient's responsibility. Billing staff create patient statements showing the services provided, insurance payment amounts, adjustments, and the balance owed. These statements are mailed to patients or made available through online patient portals.
Effective statements include clear payment instructions and options. Many providers send statements every 30 days, with some offering payment plans for larger balances. This allows patients to pay over time rather than in one lump sum, improving collection rates and patient satisfaction.
Step 8: Following Up
The final step in medical billing involves following up on unpaid claims and outstanding patient balances. For insurance claims, billing specialists contact payers about claims that remain unpaid, providing additional documentation or filing appeals for denied claims as needed.
For patient balances, follow-up includes sending additional statements, making phone calls to discuss payment options, and working with collection agencies for severely delinquent accounts. This final step often determines whether the practice collects payment or writes off the balance as bad debt, making it essential to the organization's financial health.
What are Tier 1 and Tier 2 in Medical Billing?
Tier 1 and Tier 2 in medical billing typically refer to levels of claim complexity and the expertise required to work them. This classification system helps billing departments organize workflows and assign tasks appropriately based on staff skill levels and claim difficulty.
Tier 1 claims are straightforward claims that have been paid correctly or require minimal intervention. These might include clean claims that are processed without issues, simple claim corrections, or routine patient balance follow-up. Tier 1 work is typically handled by entry-level billing staff or can often be automated through billing software. The focus at this level is on high-volume, routine tasks that follow established procedures.
Tier 2 claims are more complex and require experienced billing specialists to resolve. These include denied claims requiring appeals, claims with complex coding issues, accounts with unusual payment patterns, or situations requiring direct communication with insurance company representatives. Tier 2 billing staff need deeper knowledge of payer policies, coding guidelines, and problem-solving skills to navigate these challenging scenarios. Some organizations also use a Tier 3 designation for the most complex cases requiring senior expertise or manager involvement.
Challenges RCM Teams Face in Medical Billing Today
Revenue cycle management teams face significant obstacles that directly impact the bottom line.
Consider this: claim denials alone cost the healthcare industry an estimated $262 billion annually, with the average denial costing $118 to rework. The numbers tell a sobering story—between 5-10% of all claims are initially denied, and roughly 65% of denied claims are never resubmitted, representing pure revenue loss.
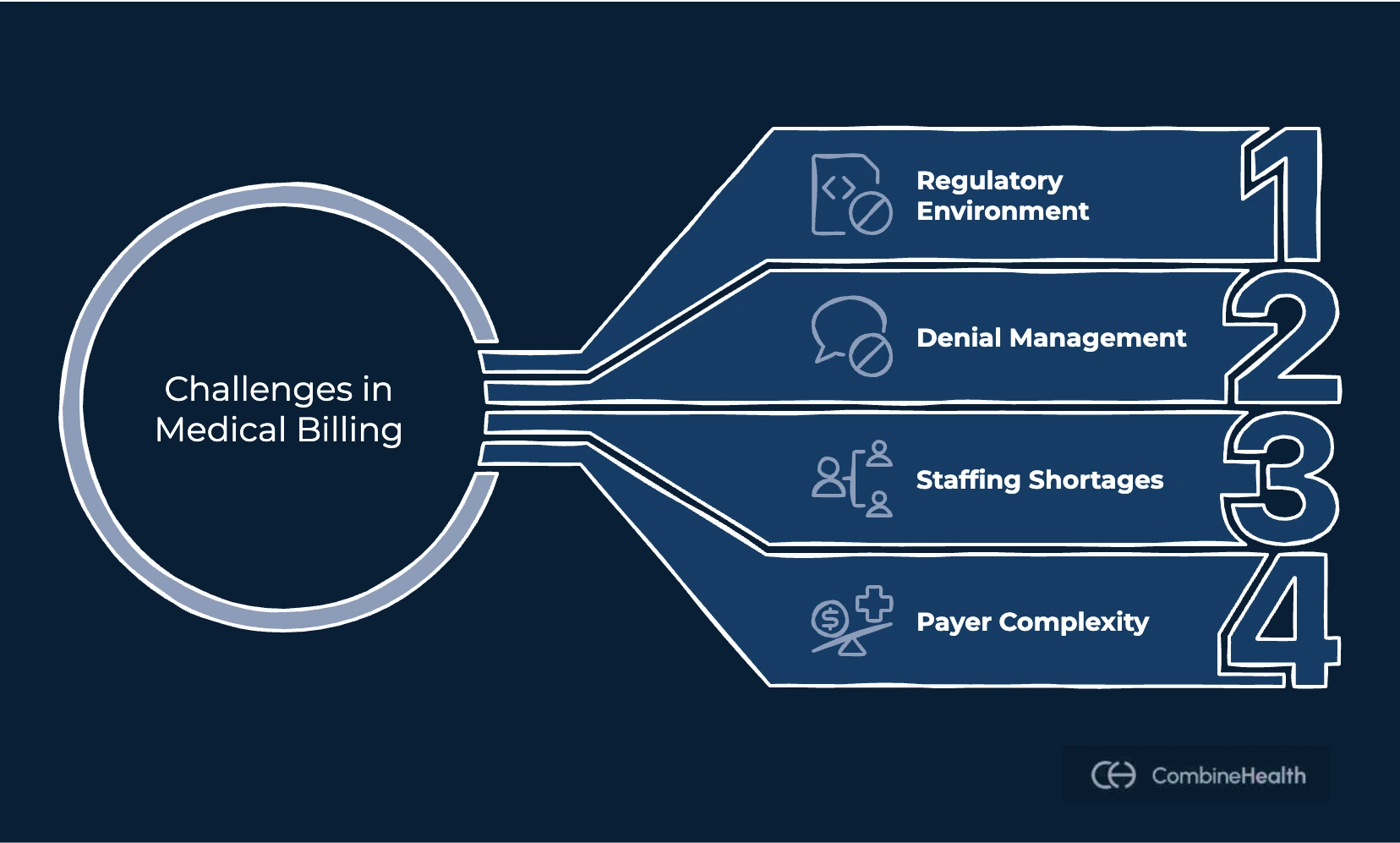
The regulatory environment compounds these challenges, with over 140,000 annual updates to medical codes and billing rules that staff must continuously learn and implement. Each denial requires an average of 20-30 minutes of staff time for research, correction, and resubmission, with many stemming from preventable errors like:
- Missing information
- Incorrect coding
- Eligibility issues that proper verification could catch upfront
Staffing shortages and payer complexity add to these difficulties. Since medical billing requires specialized knowledge, training new employees often takes months, while experienced billers are constantly recruited away.
Additionally, each insurance company maintains different policies, documentation requirements, and billing procedures. Staff must navigate hundreds of payer-specific rules, and staying current with policy changes across multiple payers proves nearly impossible.
How AI Can Help Address The Medical Billing Challenges
Artificial intelligence is emerging as a powerful tool to overcome many of the obstacles that burden medical billing departments. Here’s how it can help in medical billing:
1. Coding Automation
AI-powered coding systems, such as Amy by CombineHealth, analyze clinical documentation and suggest appropriate diagnosis and procedure codes, dramatically reducing the time coders spend on routine cases.
Natural language processing algorithms read physician notes, identify key clinical concepts, and map them to the correct codes based on official coding guidelines. These systems continuously learn from corrections, feedback, and denials, improving accuracy over time while staying current with coding updates automatically. AI is already helping organizations submit claims faster, improving cash flow, and reducing denials
2. Flagging Billing Errors
AI algorithms analyze claims before submission and flag potential errors, missing information, or compliance issues that might lead to denials. These systems check for common problems like:
- Mismatched diagnosis and procedure codes
- Missing modifiers
- Incorrect patient demographics
- Services requiring prior authorization
Machine learning models trained on historical claim data identify patterns associated with denials, learning which combinations of codes, payers, and circumstances frequently result in problems. This predictive capability allows billing teams to address issues proactively, significantly improving first-pass claim acceptance rates.
3. Claim Scrubbing
Advanced claim scrubbing powered by AI provides intelligent analysis of claim accuracy and completeness by validating against vast databases of payer policies, coding guidelines, and regulatory requirements.
These systems identify subtle issues that traditional scrubbing software might miss, such as coding combinations that are technically valid but likely to be questioned by specific payers. AI-driven scrubbing adapts to changing payer requirements automatically by monitoring claim outcomes and adjusting validation rules based on recent denial patterns, ensuring effectiveness even as payer policies evolve.
4. Payment Posting and Reconciliation
AI streamlines payment posting and reconciliation by automatically reading remittance advice documents and applying payments to correct patient accounts. Optical character recognition combined with natural language processing extracts payment information from both electronic remittances and paper EOBs, eliminating manual data entry.
Machine learning algorithms detect patterns in underpayments or incorrect adjustments, alerting billing staff to systematic issues with specific payers or procedure codes and helping organizations identify revenue leakage faster than manual review allows.
5. Claim Processing
AI accelerates overall claim processing by orchestrating the various steps required to move from service delivery to payment. Intelligent workflow systems route claims to appropriate staff based on complexity, automatically escalate issues requiring attention, and prioritize work queues based on factors like claim age, dollar value, and likelihood of success. Predictive analytics forecast claim payment timelines and identify accounts likely to require follow-up, allowing billing teams to allocate resources proactively and helping managers optimize staffing while setting realistic expectations for revenue realization.
CombineHealth's AI Agent Mark assists medical billing teams by automating eligibility verification, claim status checking, and denial management workflows. Mark integrates directly with payer portals and EHR/PMS to handle routine inquiries, freeing staff to focus on complex cases that require human judgment. By reducing manual workload and accelerating routine processes, CombineHealth helps organizations improve their revenue cycle performance while containing costs.
What Are the Benefits of Using AI for Medical Billing?
Enhanced Accuracy and Speed
AI systems reduce human error by consistently applying coding guidelines, payer policies, and validation rules across thousands of claims while completing tasks like coding, claim scrubbing, and payment posting in seconds rather than minutes. This combination of accuracy and speed translates to faster claim submission, shorter revenue cycles, improved cash flow, and significant reductions in claim denial rates and billing errors that directly improve revenue.
Reduced Denials
By identifying and correcting potential issues before claims reach payers, AI significantly reduces denial rates by 20-40%. Fewer denials mean less rework, faster payment, and better financial performance while creating a more positive work environment for billing staff.
Improved Compliance and Audit Readiness
AI systems maintain detailed logs and comprehensive audit trails showing how decisions were made and what information supported each claim. The consistent application of coding and billing rules reduces compliance risk while proactive monitoring helps organizations avoid costly violations and penalties.
Better Patient Experience
AI improvements benefit patients through more accurate billing, faster resolution of insurance issues, and clearer explanations of financial responsibility. AI-powered communication tools provide personalized payment options and 24/7 support, contributing to overall satisfaction and increasing the likelihood that patients will pay their balances.
Ready To Streamline Your Medical Billing Processes?
Medical billing remains one of healthcare's most essential yet challenging administrative functions, requiring detailed knowledge of coding, payer policies, and complex regulations. As healthcare becomes increasingly complex and patients shoulder more financial responsibility, the importance of efficient, accurate billing grows.
Artificial intelligence offers powerful solutions to many longstanding medical billing challenges. By automating routine tasks, flagging potential errors, and augmenting human capabilities, AI enables billing departments to process more claims with greater accuracy and speed.
If you’re wondering how CombineHealth’s billing solution Mark can help you with your medical billing workflows, book a demo!
FAQs
What is medical billing, and why is it important?
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for healthcare services, ensuring providers are compensated for care, and maintaining the financial viability of medical practices.
What is an EOB in medical billing?
An Explanation of Benefits (EOB) is a statement sent by insurance companies to patients after processing a claim, explaining what services were billed, how much insurance paid, and what the patient owes.
What is a grace period in medical billing?
A grace period in medical billing is a timeframe during which a payment is still considered on time even if received after the due date, or when insurance coverage remains active despite a missed premium payment (typically 90 days for marketplace plans).
What is RCM in medical billing?
Revenue Cycle Management (RCM) encompasses all administrative and clinical functions that contribute to capturing, managing, and collecting patient service revenue, from patient registration through final payment collection.
What is a TPI number in medical billing?
A TPI number (Taxpayer Identification Number) is a unique identifier assigned to healthcare providers for billing and tax purposes, required by insurance companies to properly identify billing entities and ensure payment reaches the correct provider.
What is an entity code in medical billing?
An entity code is a two-character alphanumeric identifier used in electronic medical billing transactions to specify what type of entity is being referenced, such as the patient, insured subscriber, rendering provider, or billing provider.
What is capitation in medical billing?
Capitation is an alternative payment model where providers receive a fixed amount per patient per time period (usually monthly), regardless of services used, shifting financial risk from payers to providers and incentivizing preventive care.
What are Tier 1 and Tier 2 in medical billing?
Tier 1 and Tier 2 refer to levels of claim complexity, with Tier 1 representing straightforward claims handled by entry-level staff or automation, and Tier 2 involving complex claims requiring experienced billing specialists.
What is ERA in medical billing?
Electronic Remittance Advice (ERA) is the electronic version of payment information sent from insurance companies to healthcare providers, detailing which claims were paid, adjusted, or denied, along with reason codes and payment amounts.
What is a superbill in medical billing?
A superbill is a detailed document that itemizes all services provided during a patient encounter, including demographics, diagnosis codes, procedure codes, and charges, serving as the source document for creating insurance claims.
What is a clearinghouse in medical billing?
A clearinghouse acts as an intermediary between healthcare providers and insurance payers, receiving claims, checking them for errors, formatting them according to payer specifications, and electronically transmitting them to appropriate insurance companies.
What is unbundling in medical billing?
Unbundling is the improper practice of billing separately for procedures that should be billed together as a single comprehensive service, considered a compliance violation because it results in higher payment than appropriate.
What is the minimum monthly payment on medical bills?
There is no universally mandated minimum monthly payment for medical bills, though many healthcare providers accept payments as low as $25-50 per month based on a patient's financial situation through negotiated payment plans.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai







.png)









