MIPS Healthcare: What It Is, Why It Costs You Money, and How to Implement It Effectively
Discover what MIPS Healthcare is, why it impacts your Medicare reimbursements, and how to implement it effectively to avoid penalties and maximize performance.
October 9, 2025


Key Takeaways:
• MIPS Healthcare, part of the Merit-Based Incentive Payment System, directly ties Medicare reimbursement to quality, cost, and interoperability performance.
• Missing the 75-point performance threshold in the Based Incentive Payment System can trigger up to a 9% payment penalty.
• Common score killers in MIPS Healthcare include documentation gaps, coding errors, and missed reporting deadlines.
• Treat the MIPS Healthcare program as a continuous improvement system — monthly tracking and automation are key to unlocking positive adjustments.
Medicare reimbursements are tied to performance under the MIPS Healthcare program, also known as the Merit-Based Incentive Payment System (MIPS). Under MIPS, your payment adjustments can range up to +9% or -9%, depending on how well your practice performs.
And yet, most organizations still treat MIPS as a year-end compliance task instead of a financial strategy.
This guide breaks down what MIPS actually is, how it works, why it’s costing you money, and how to implement it effectively.
What Is MIPS in Healthcare?
The Merit-Based Incentive Payment System (MIPS Healthcare program) is a CMS program that ties Medicare Part B reimbursement to the quality, cost, and efficiency of care you deliver. Introduced under the Medicare Access and CHIP Reauthorization Act (MACRA), MIPS replaced legacy programs like PQRS and Meaningful Use.
Its goal is simple: to reward providers who deliver high-quality, cost-efficient care, and penalize those who don’t.
MIPS is part of the broader Alternative Payment Model (APM) Framework, meaning it’s a stepping stone toward value-based care. Each year, CMS calculates a final performance score for every eligible clinician or group—that score then determines your Medicare payment adjustment two years later.
In 2025, the MIPS performance threshold remains 75 points, with potential adjustments of +9% to -9% based on how your score compares to national benchmarks.
Also read: Other payment models in healthcare delivery, such as fee-for-service and value-based care
Why It Matters
For most organizations, MIPS is no longer optional. If a clinician or group meets MIPS eligibility but does not participate or achieves a performance score below the annual threshold (75 points for 2025), they can receive penalties of up to -9% on Medicare payments.
Also, if you bill more than $90,000 in Medicare Part B, serve 200 or more beneficiaries, and provide 200 or more covered professional services, you’re eligible for MIPS. Failing to comply can directly cut your bottom line.
How Does MIPS Work?
Understanding how the MIPS Healthcare program works is essential before optimizing it. The Merit-Based Incentive Payment System evaluates clinical quality, efficiency, and interoperability across key performance categories.
The Four MIPS Performance Categories
MIPS Reporting
Here are the step-by-step guidelines for MIPS reporting:
1. Check Your Eligibility
Use the CMS QPP Participation Status Tool to confirm if you or your group must participate. Remember: eligibility is reassessed twice annually.
2. Select Reporting Option
Choose whether to report as an individual, group, or APM entity. Group reporting can smooth out outliers but requires better coordination.
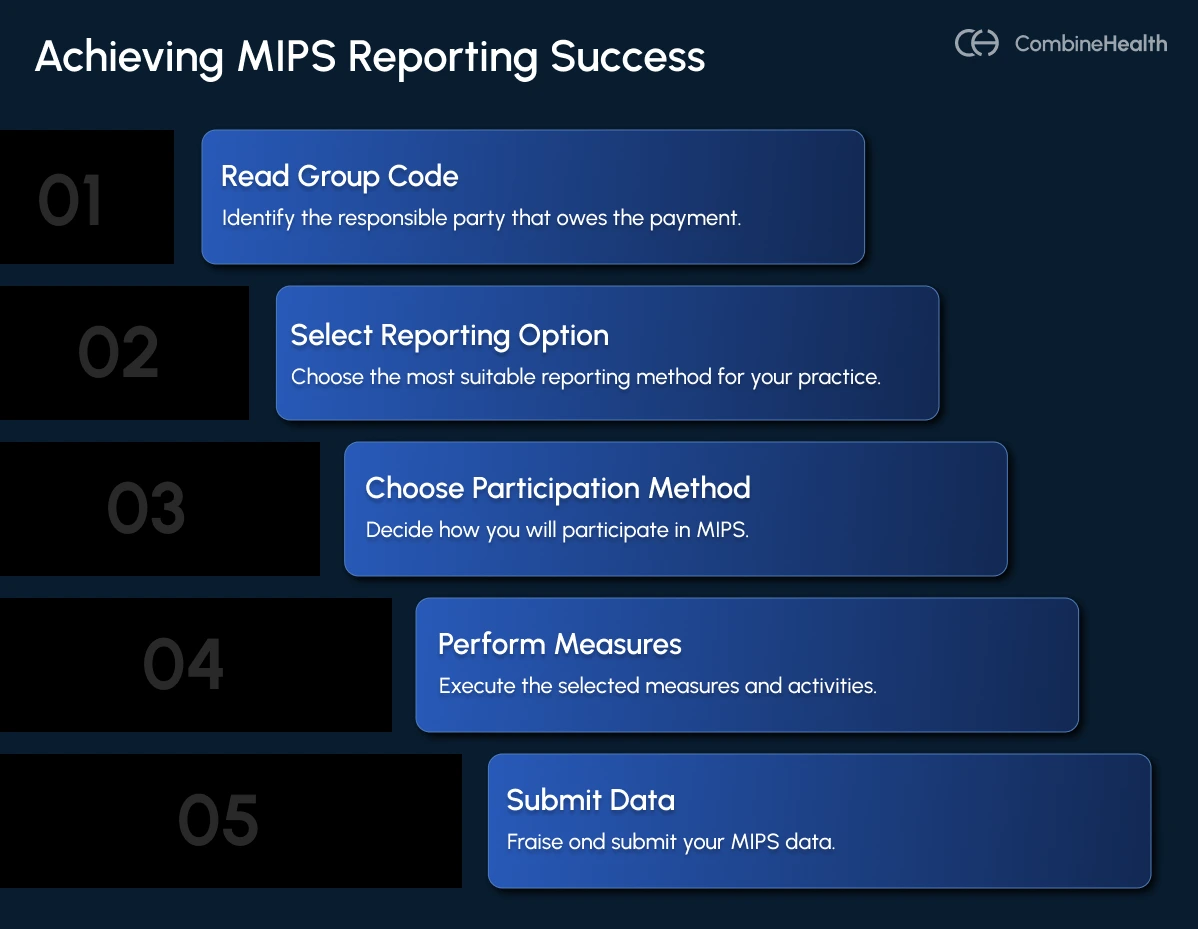
3. Choose Your Participation Method
Traditional MIPS or MIPS Value Pathways (MVPs). MVPs bundle related measures by specialty (e.g., dermatology, cardiology) and simplify selection.
4. Select and Perform Your Measures and Activities
Pick the measures that best match your practice type and case mix. Underperforming or irrelevant measures can drag your score down.
5. Submit Your Data
Report via your EHR, a qualified registry (QCDR), or CMS portal before the deadline — typically March 31 following the performance year.
Scoring and Payment Adjustment
Your final MIPS Healthcare score determines a payment adjustment applied two years later under the Merit-Based Incentive Payment System.
How MIPS Penalties Can Impact Your Revenue
MIPS is budget-neutral. This means every bonus paid to a high performer is funded by penalties from underperformers.
So when your data isn’t clean, your technology isn’t configured, or your team misses details, you’re not just losing points—you're funding someone else’s bonus.
Let’s look at the financial impact and root causes:
- A clinic billing $3M in Medicare Part B can lose $270,000 with a -9% penalty.
- Even a -2% adjustment equals $60,000 — often more than the cost of your billing team.
- Many groups don’t realize they missed the performance threshold until it’s too late, because CMS feedback loops are delayed by 18–24 months.
These hidden losses compound year after year.
Operational Failures That Lead to Low MIPS Scores

1. Documentation Gaps
Incomplete clinical documentation, missing encounter details, or unsupported diagnoses lower your quality and cost performance.
Example:
A provider documents “chest pain” without specifying “unstable angina,” missing an HCC code, and reducing accuracy.
2. Measure Mismatch
Selecting measures unrelated to your case mix dilutes your score.
Example:
A neurology clinic reporting primary care preventive metrics will almost always underperform.
3. Credentialing and Enrollment Slips
Expired payer enrollments or incorrect NPIs lead to denials, reducing net revenue and impacting MIPS cost efficiency.
4. Coding Errors or Undercoding
Incorrect CPT/ICD-10 codes affect both cost and quality.
Example:
Undercoding chronic conditions lowers risk adjustment and drags down quality scores.
5. Promoting Interoperability (PI) Failures
If your EHR isn’t configured properly or if your staff forgets to enable certain PI measures, your entire category can be reweighted or scored zero.
Use AI solutions that integrate directly into your EHR and help monitor whether data exchange and patient portal metrics meet CMS thresholds automatically.
6. Poor Evidence Collection
During audits, missing screenshots, log files, or attestation documentation can cost points. Modern compliance assistants can retrieve CMS policy references or payer rules with page-level citations, strengthening your audit defense.
7. Small-Practice Resource Limits
Limited staff means less time for quality tracking, reporting, and data validation. A single misreported measure can reduce your score by 5–10 points.
How to Implement MIPS Effectively
The MIPS Healthcare framework is complex, but it’s manageable when treated like a continuous performance management system. Whether you’re new to the Merit-Based Incentive Payment System or refining existing workflows, structured governance and automation are the foundation of compliance.
Below is a practical roadmap for healthcare organizations to stay above the 75-point threshold consistently:
1. Establish Governance Early
Assign a MIPS lead (often your compliance officer or RCM manager) to own performance tracking. Hold monthly reviews on category performance, data completeness, and cost trend analysis.
Also read: How AI is used in healthcare and how it’s different from automation
2. Automate Quality and Cost Tracking
Don’t wait for CMS feedback 18 months later. Instead, use internal dashboards or automation platforms to track the following key metrics monthly:
- Denial rate
- Average cost per beneficiary
- Quality measure completeness
This real-time insight allows you to intervene early, even before the MIPS penalties accrue.
3. Choose the Right Measures
Focus on measures you can control and document consistently.
For 2025, CMS encourages adoption of MIPS Value Pathways (MVPs), structured around clinical specialties and outcomes.
Example:
A cardiology practice might select the “Heart Disease Prevention and Management” MVP, aligning directly with its care delivery data.
4. Leverage Technology for Evidence and Compliance
Manual data collection is inefficient and error-prone. Integrate AI solutions that can help in instantly retrieving payer-specific coverage criteria and ensure proper coding alignment with quality measures. Every data point submitted should be defensible, explainable, and audit-ready.
5. Integrate With EHR and Billing Systems
Disconnected workflows create reporting blind spots. Solutions that plug directly into your EHR can capture structured data automatically, ensuring 100% completeness across encounters.
CombineHealth’s AI agents work within your existing billing software, automating charge entry, claim submission, and documentation validation.
6. Continuous Staff Education
MIPS rules evolve annually. Hold quarterly training sessions for clinicians, coders, and billers on updated measure definitions, topped-out scores, and new cost calculation methodologies. Encourage staff to review CMS updates or leverage AI training assistants to summarize relevant rule changes in simple language.
Also read: AI governance in healthcare for ensuring responsible use of technology
7. Monitor Cost Drivers
The Cost category is fully claims-based, meaning you can’t fix it at submission time.
That’s why it’s advised to proactively monitor:
- High-cost episodes
- Readmission trends
- Referral patterns
Use cost analytics to identify where resource use exceeds benchmarks, then target interventions.
8. Audit and Review Before Submission
Two months before the submission deadline, conduct an internal audit. Ensure:
- All measures meet completeness thresholds
- Documentation supports reported performance
- Attestations for Promoting Interoperability are backed by evidence
The Future of MIPS: MVPs and Value-Based Care
CMS is signaling a gradual shift from Traditional MIPS Healthcare reporting to MVPs (MIPS Value Pathways), evolving the Based Incentive Payment System toward specialty-specific outcomes.
By 2026–2027, traditional reporting may sunset entirely, replaced by MVPs aligned to clinical specialties and outcomes.
Organizations that standardize data capture, automate performance tracking, and integrate compliance intelligence early will be better positioned for that transition.
AI-driven RCM platforms, like CombineHealth’s multi-agent AI workforce, are already being used to align coding accuracy, documentation integrity, and payer compliance under one roof.
The good news: the same AI automation that’s transforming RCM can make MIPS performance predictable, auditable, and profitable. By automating coding, documentation, payer policy checks, and denial analytics, practices can move from penalty avoidance to performance optimization.
The payoff: higher reimbursements, fewer claim denials, and the confidence that every Medicare dollar you’ve earned actually reaches your account.
Book a demo with CombineHealth today!
FAQs
What does MIPS mean in healthcare?
MIPS in healthcare stands for Merit-based Incentive Payment System. It’s a program that links Medicare payments to provider performance based on quality, cost, improvement activities, and interoperability. The goal is to encourage high-quality, efficient, and patient-centered care.
What is MIPS used for in healthcare?
MIPS, or the Merit-Based Incentive Payment System, is used in healthcare to evaluate clinicians’ performance based on quality, cost, improvement activities, and interoperability. It adjusts Medicare payments to encourage high-quality, efficient, and patient-centered care while reducing costs and improving overall healthcare outcomes.
Who is eligible for MIPS?
Eligible clinicians for MIPS include physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists who bill Medicare Part B. To qualify, they must exceed low-volume thresholds based on Medicare patients, services, and allowed charges during the performance year.
What happens if I don't participate in MIPS?
If you don’t participate in MIPS, you may face up to a 9% penalty on your Medicare reimbursements. Non-participation also means missing out on potential positive payment adjustments and the opportunity to improve care quality and performance reporting under the Medicare program.
Is MIPS for Medicaid?
No, MIPS is not for Medicaid. The Merit-Based Incentive Payment System (MIPS) applies only to clinicians billing Medicare Part B. However, some Medicaid programs may have their own quality reporting or value-based incentive initiatives that operate separately from MIPS.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)










