Medical Coding Audit: A Step-by-Step Guide to Reduce Denials
Learn how to perform a medical coding audit step by step to improve accuracy, ensure compliance, and reduce claim denials with smarter workflows.
February 16, 2026


Key Takeaways:
• Medical coding audits help reduce denials by identifying documentation gaps and coding inconsistencies early.
• Structured audit workflows improve compliance and revenue cycle performance.
• Risk-based sampling ensures audits focus on high-impact areas.
• Combining documentation review with coding validation strengthens accuracy.
• AI-assisted tools help scale audits by identifying patterns and risks earlier.
A medical coding audit is like a diagnostic scan for your revenue cycle — it reveals hidden issues before they turn into bigger financial or compliance problems. Although claims may appear to move smoothly through the system, small gaps in documentation, incorrect modifiers, or payer rule mismatches can quietly increase the risk of denials and slow reimbursements.
About 60% of medical groups reported claim denials being higher in 2024 than in the previous year. More denials create significant administrative rework and disrupt revenue. A structured healthcare coding and compliance audit helps teams identify these risks early by validating coding accuracy, reviewing documentation, and ensuring compliance with evolving payer rules.
In this guide, you’ll learn how to conduct effective medical coding audits step by step and how AI-assisted tools can help teams identify gaps sooner, turning audits from reactive checks into proactive workflows.
What Is a Medical Coding Audit?
A medical coding audit is a structured review of clinical documentation and coded claims to ensure that coding accurately represents the services delivered and meets payer requirements. The goal is to verify coding accuracy, confirm compliance with payer and regulatory requirements, and identify patterns that may lead to denials or revenue leakage.
In many healthcare organizations, this process is integrated into a broader medical claims audit strategy to ensure both clinical and financial accuracy.
Unlike routine claim checks, a coding audit looks beyond individual errors. It involves examining workflows, documentation practices, coding decisions, and internal coding procedures to uncover systemic issues, like:
- Inconsistent modifier usage
- Undercoding or upcoding trends
- Documentation gaps
These issues can prevent claims from meeting medical necessity requirements. This allows organizations to address root causes rather than repeatedly fix the same problems.
How Does Medical Coding Work?
The medical coding audit process typically involves comparing encounter notes against Current Procedural Terminology (CPT) codes, International Classification of Diseases (ICD) diagnosis codes, and Evaluation and Management (E/M) level selection.
Auditors also review payer-specific guidelines and evaluate whether documentation supports the level of service billed. Depending on organizational needs, audits may focus on compliance risk, revenue optimization, denial reduction, or coder education.
Regular audits also help teams stay aligned with constantly evolving coding standards and payer policies. As guidelines change and reimbursement models shift, even experienced coders can benefit from structured reviews that reinforce best practices and maintain consistency across the revenue cycle.
Why Medical Coding Audits Are Important
Medical coding audits do more than just check compliance. They protect revenue, improve operational efficiency, and strengthen documentation quality across the organization. Here’s what they help with:
Reduce Preventable Claim Denials
Many denials stem from issues that audits can catch early, such as missing documentation elements, incorrect coding, incorrect modifiers, or mismatches between diagnosis and procedure codes. By identifying patterns in rejected claims, teams can correct workflows before errors repeat, improving first-pass acceptance rates and reducing rework.
Maintain Compliance With Evolving Payer Rules
Coding guidelines and payer policies change frequently. Regular audits help ensure coding practices remain aligned with current updates, payer-specific requirements, and regulatory expectations. This reduces compliance risk and helps organizations prepare for external audits with greater confidence.
Improve Documentation Quality
Audits often reveal gaps between clinical documentation and coding decisions. These insights allow teams to educate healthcare providers on documentation best practices, ensuring medical necessity is clearly supported, thus reducing ambiguity during claim review.
Strengthen Revenue Cycle Performance
Accurate coding directly impacts reimbursement outcomes. By identifying undercoding, overcoding, or missed billing opportunities, audits help organizations optimize revenue integrity while maintaining compliance standards. Optimizing audits also strengthens the broader coding and billing process, ensuring smoother reimbursement cycles.
Types of Medical Coding Audits
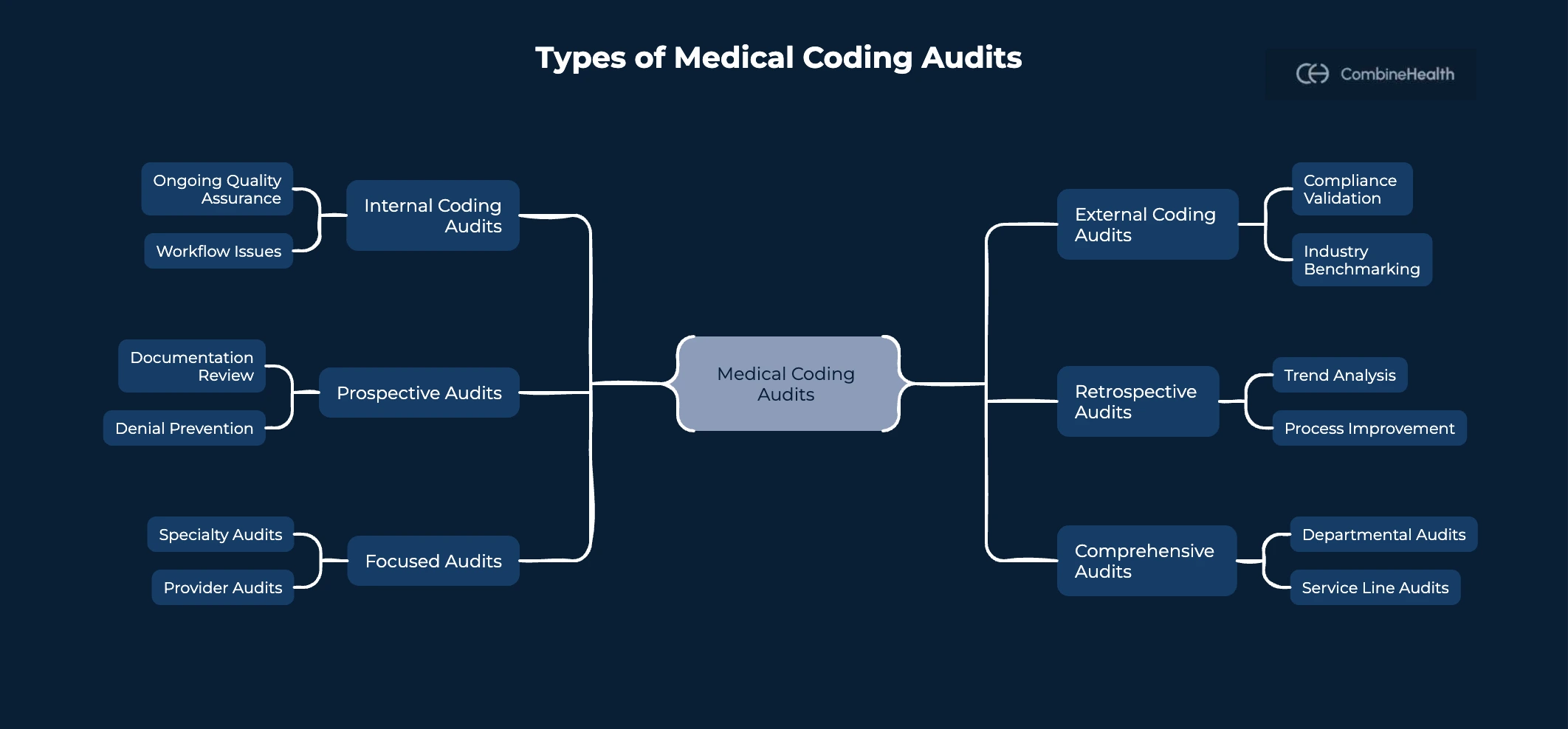
Not all medical coding audits serve the same purpose. Organizations typically choose an audit type based on their goals, whether to improve compliance, identify denial patterns, or validate coding accuracy before claim submission. Here are the different types of medical coding audits:
Internal Coding Audits
Internal audits are conducted by in-house coding teams or compliance staff. These audits focus on ongoing quality assurance, helping organizations monitor coding accuracy, identify workflow issues, and reinforce internal standards. Because they occur regularly, internal audits help teams detect problems early and make continuous improvements.
External Coding Audits
External audits are performed by independent auditors or third-party specialists. These reviews provide an objective assessment of coding practices and are often used to validate compliance, prepare for regulatory reviews, or benchmark performance against industry standards. External audits can also uncover blind spots that internal teams may overlook. Many healthcare organizations also engage specialized coding audit services to ensure objective performance validation.
Based on timing, medical coding audits can also be categorized as Prospective and Retrospective audits:
Similarly, based on scope and objective, medical coding audits can also be categorized as Focused and Comprehensive audits.
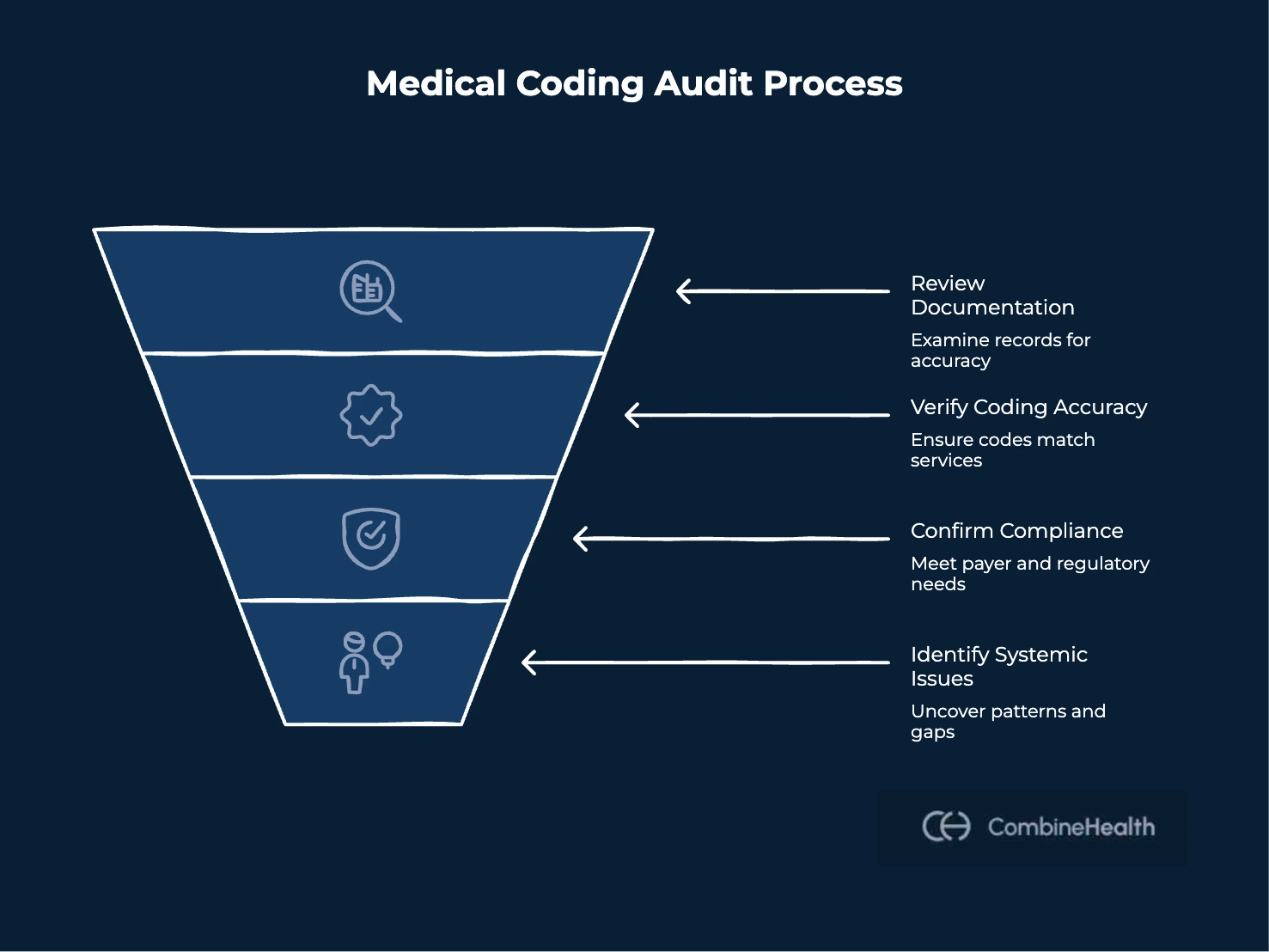
Step-by-Step Process to Perform a Medical Coding Audit
The following framework outlines how organizations can conduct effective audits that reduce denial risk and improve coding accuracy over time.
Step 1: Start by Defining Clear Audit Objectives and Scope
Every audit should begin with a clear understanding of what the organization wants to achieve. Establishing the scope early helps ensure the audit remains targeted and efficient. Determine:
- The specialties, providers, or departments that will be included
- Whether the audit will be prospective or retrospective
- Any known risk areas, such as frequently denied codes or recently updated procedures
Many healthcare organizations reference a standardized medical coding audit checklist during this phase to ensure objective alignment and evaluation consistency.
Clear objectives help guide sampling, evaluation criteria, and reporting outcomes.
Step 2: Select a Representative Sample of Charts Based on Risk and Performance Data
Rather than selecting samples without context, organizations should use structured sampling methods that reflect real risks. A balanced sample improves the accuracy of audit conclusions. Common approaches include:
- Random sampling to assess overall coding quality
- Targeted sampling based on denial trends or payer feedback
- Provider-specific sampling when performance differences are suspected
Using data-driven sampling ensures the audit identifies meaningful patterns instead of isolated issues.
Step 3: Review Clinical Documentation to Confirm Completeness and Clarity
Before evaluating coding accuracy, auditors should assess whether clinical documentation fully supports the services billed. Missing or unclear documentation is one of the most common reasons for coding discrepancies. Look for:
- Incomplete procedure descriptions
- Missing findings or supporting details
- Lack of specificity required for accurate coding and medical necessity validation
Identifying documentation gaps early helps prevent downstream coding errors.
Step 4: Evaluate Coding Accuracy Against Documentation and Guidelines
Once documentation quality has been confirmed, compare clinical notes against assigned codes to determine whether they accurately reflect the services provided and follow established medical coding procedures. This includes reviewing:
- Current Procedural Terminology (CPT) code selection
- International Classification of Diseases (ICD) diagnosis coding
- Evaluation and Management (E/M) level determination
- Modifier usage and sequencing
Instead of focusing only on individual mistakes, look for recurring patterns that suggest workflow or training issues.
Step 5: Assess Compliance with Payer Rules and Policy Requirements
Coding accuracy alone does not guarantee successful reimbursement. Each payer may apply different coverage policies, documentation expectations, and billing rules.
Evaluating compliance with these requirements helps identify potential denial risks before claims are submitted or appealed.
Step 6: Analyze Findings to Identify Trends and Root Causes
After reviewing individual charts, aggregate the results to uncover systemic issues. Trends may include persistent documentation gaps, misunderstandings in coding related to updated guidelines, or workflow problems affecting multiple team members. These findings often reveal weaknesses in the overall medical coding process that require structured improvements.
Root cause analysis helps organizations address underlying problems instead of repeatedly correcting the same errors.
Step 7: Document Audit Results and Establish Feedback Loops for Improvement
A coding audit delivers value only when findings translate into action. Summarize results clearly and share insights with coding teams, billers, and providers. Include:
- Error categories and frequency
- Compliance risks identified
- Training or education opportunities
- Recommended workflow improvements
Creating structured feedback loops ensures audits drive continuous improvement rather than remaining one-time exercises.
Challenges Teams Face When Conducting Medical Coding Audits
Maintaining consistency in conducting medical coding audits is challenging, even when organizations understand its significance. Some of the common challenges are:
Limited Time and Staffing Resources
Coding teams are often managing high claim volumes alongside daily operational responsibilities. Conducting thorough audits requires dedicated time, which many organizations struggle to allocate. As a result, audits may be rushed or performed less frequently than needed.
Rapidly Changing Coding and Payer Requirements
Coding standards and payer policies evolve frequently. Keeping audit criteria aligned with updated CPT guidelines, ICD updates, and payer-specific rules can be challenging without structured processes.
Fragmented Data Across Systems
Clinical documentation, coding workflows, payer communications, and denial data often exist in separate systems. This fragmentation makes it difficult to gather all relevant information during audits, slowing the review process and increasing the risk of missed insights.
Identifying Patterns at Scale
Manual audits typically focus on small chart samples, making it harder to detect broader trends, such as recurring documentation gaps or systemic coding inconsistencies. Without scalable analysis, organizations may address symptoms rather than root causes.
However, the good news is that you can solve all these challenges by effectively implementing artificial intelligence (AI) tools.
How AI Improves Medical Coding Audits
Traditional medical coding audits rely heavily on manual review, which can limit scalability and delay insights. As coding requirements become more complex and payer policies evolve frequently, AI can help organizations strengthen audit processes by improving efficiency, consistency, and early risk detection.
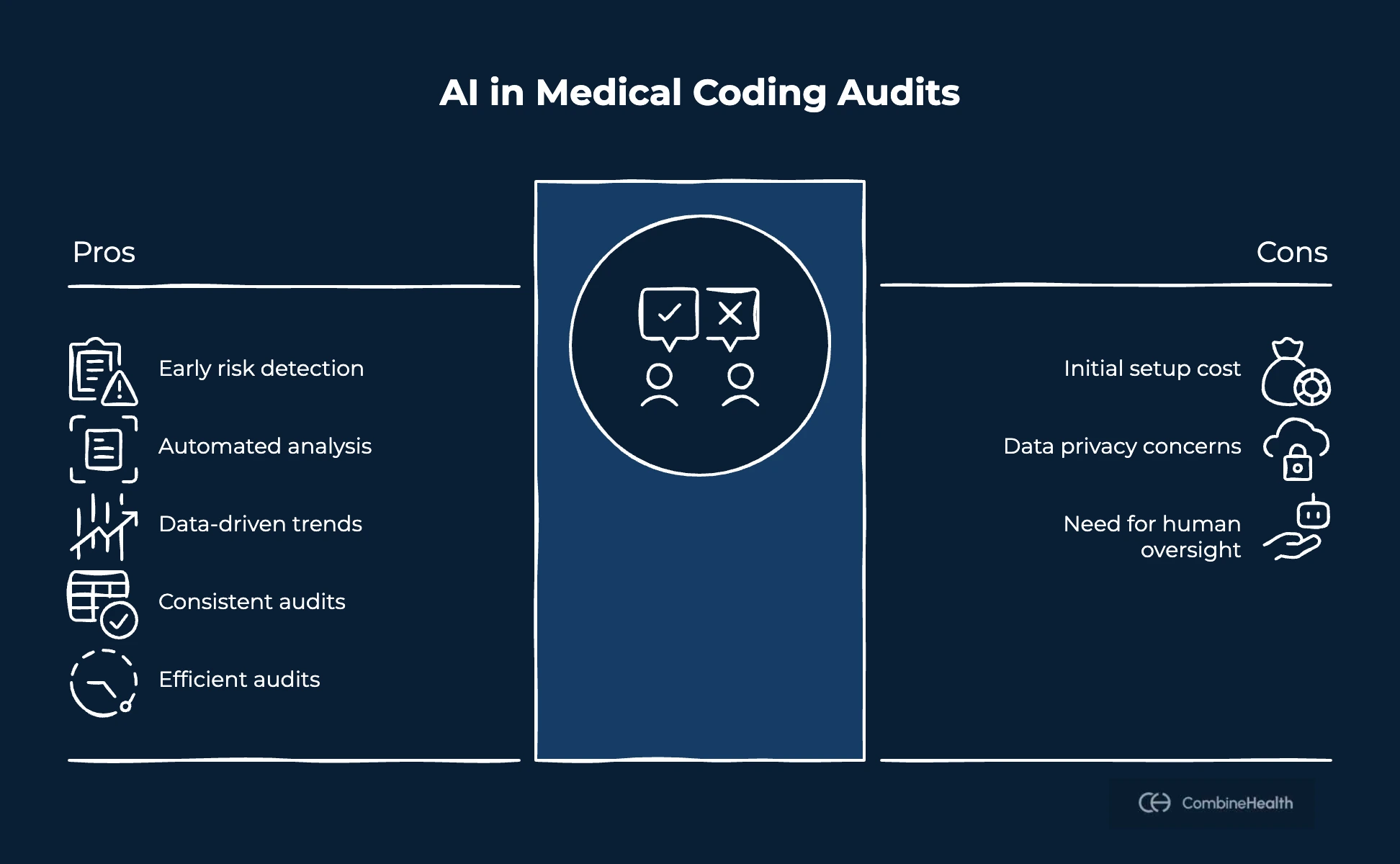
Earlier Risk Identification
AI tools can analyze clinical documentation and coding patterns before claims are submitted. This allows teams to identify potential discrepancies, missing information, or coding risks earlier, helping reduce downstream denials and rework.
In this context, CombineHealth’s AI medical coding solution, Amy, automates early risk detection by reviewing encounter documentation directly from EHR systems and validating coding decisions against clinical context. By suggesting appropriate CPT codes, ICD diagnoses, and E/M levels while sequencing diagnoses correctly, Amy helps teams identify potential issues before submission rather than during retrospective audits.
Automated Documentation Analysis
Reviewing documentation manually across multiple encounters can be time-consuming. AI systems can scan clinical notes at scale and highlight areas where documentation may not fully support coding decisions or medical necessity requirements, enabling faster and more thorough reviews.
Amy supports this workflow by analyzing documentation line by line and flagging gaps such as incomplete procedure descriptions, missing clinical findings, or insufficient justification for medical necessity. This allows auditors and coders to focus on high-risk areas instead of manually reviewing every chart in detail.
Data-Driven Trend Analysis
AI can analyze larger datasets than manual audits typically allow. By identifying patterns across providers, specialties, or coding categories, AI helps organizations uncover systemic issues rather than focusing only on isolated errors.
Amy contributes by reviewing multiple charts simultaneously and surfacing recurring coding patterns or documentation risks across providers or service lines. This enables organizations to identify training opportunities or workflow changes that prevent repeat errors.
Improved Consistency and Audit Efficiency
Standardizing audit criteria manually can be difficult across large teams. AI supports consistency by applying structured review logic across cases, helping auditors maintain uniform evaluation standards while reducing repetitive manual work.
Operating within a human-in-the-loop workflow, Amy provides coding recommendations alongside detailed rationale explaining how documentation supports each coding decision. This transparency allows auditors to maintain oversight while expanding audit coverage more efficiently. Typically, Amy reviews a chart in approximately two to four minutes and helps teams scale auditing workflows without sacrificing accuracy.
Best Practices for Building an Ongoing Medical Coding Audit Program
Conducting occasional audits can help identify individual errors, but long-term success comes from building a structured and repeatable audit program. Establishing clear processes ensures coding audits contribute to continuous improvement rather than becoming one-time compliance tasks.
Establish a Consistent Audit Schedule
Regular audits help organizations monitor coding quality over time and identify trends before they escalate. Depending on claim volume and risk level, teams may conduct monthly, quarterly, or targeted audits aligned with specific operational goals.
Use a Risk-Based Auditing Approach
Instead of reviewing charts randomly, prioritize areas with higher risk. This may include frequently denied codes, new procedures, specific providers, or specialties experiencing higher variability. Risk-based auditing helps teams focus resources where they can have the greatest impact.
Combine Documentation Review with Coding Validation
Effective audits evaluate both clinical documentation and coding decisions together. Ensuring documentation supports medical necessity and coding selection reduces the likelihood of recurring denials and strengthens compliance.
Provide Clear Feedback and Ongoing Education
Audit findings should translate into actionable insights for coders and providers. Structured feedback, training sessions, and updated guidelines help reinforce best practices and improve consistency across teams.
Leverage Technology to Support Scalability
As organizations grow, manual auditing alone may not keep pace with increasing claim volumes. Using technology tools alongside human expertise helps expand audit coverage, identify trends faster, and maintain consistency without increasing workload significantly.
Turning Medical Coding Audits Into a Proactive Workflow
Medical coding audits deliver the most value when they move beyond periodic compliance checks and become part of the everyday workflow. By combining structured audit processes with proactive documentation review and coding validation, organizations can identify risks earlier and reduce avoidable rework across the revenue cycle.
As coding complexity and payer expectations continue to evolve, many teams are shifting toward technology-supported auditing that surfaces issues before claims are submitted. AI-assisted tools like CombineHealth’s Amy help strengthen this approach by highlighting documentation gaps and supporting coding accuracy, allowing auditors to focus on decision-making while maintaining human oversight.
To explore how CombineHealth’s Amy supports medical coding audits, you can book a demo!
FAQs
How often should a medical coding audit be performed?
Most organizations conduct audits quarterly, with more frequent reviews for high-risk areas or new services.
Who should conduct medical coding audits?
Internal coding teams, compliance staff, or external auditors, depending on audit goals and resources.
What is included in a medical coding audit checklist?
Documentation review, CPT and ICD validation, E/M level checks, modifier review, and payer compliance verification.
A comprehensive medical coding audit checklist typically includes documentation review, CPT and ICD validation, E/M level checks, modifier review, payer compliance verification, and medical claims audit alignment.
Can medical coding audits help reduce claim denials?
Yes. Audits identify coding errors and documentation gaps early, helping prevent avoidable denials.
Can artificial intelligence replace human coding audits?
No. AI supports analysis and risk detection, but human expertise is required for review and final decisions.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















