How Emergency Medicine Has Evolved Over Time—and Why AI Is Its Next Great Leap Forward
Learn how AI is transforming emergency medicine documentation, coding, and billing after decades of change in the field.
October 27, 2025

.png)
Caral’s fascination with emergency medicine began long before she entered the industry.
In high school, she helplessly witnessed a severely injured boy waiting hours for care. That memory stayed with her—and shaped her lifelong focus on improving emergency systems.
Years later, while working as a writer for an emergency physician, she found herself immersed in a world that was still finding its footing.
From those early years of billing being done on typewriters and handwritten medical charts to AI being used to analyze charts and support medical necessity, Caral has seen it all. She has watched emergency medicine evolve over decades—from a reactive practice into a structured, data-driven specialty.
For this blog post, we sat down with Caral Edelberg, Chairman and Founder of Edelberg Associates, to get insights on the evolution of emergency medicine through the lens of documentation, coding, and compliance. She reflects on how the field took shape, the business challenges that defined its early years, and why the next phase of progress will depend on how effectively we pair human expertise with intelligent automation.
The Evolution of Emergency Medicine Through the Years
Some of the early emergency physicians often referenced the concept of triage—a system that took shape during the Vietnam War, when medics had to make split-second decisions about who could be saved, who needed to wait, and who couldn’t be helped. Those battlefield principles of prioritization later became foundational to modern emergency medicine.
Back in the 1960s and early 70s, there were no academic programs or formal training for emergency physicians. Hospitals billed emergency services as a flat fee, lumping them together as “Emergency Care.” Physicians were paid a percentage of what hospitals collected, with little visibility into what was actually being billed or paid.
Managing missing charts was another constant struggle. Back then, there was no HIPAA and very little concern about data privacy or record management. Doctors frequently misplaced charts, assuming no one else would need to review them.
.png)
To make matters worse, most charts were handwritten, often with barely legible notes that made it difficult to decipher what care had been provided. So, any missing or unclear information directly affected reimbursement. Eventually, the industry started to move toward carbon-copy forms, allowing multiple records to be created and shared more reliably.
That changed in the 1980s.
The Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 required separate provider numbers and billing, marking a turning point for emergency medicine. For the first time, physicians had to track their own performance, charges, and collections.
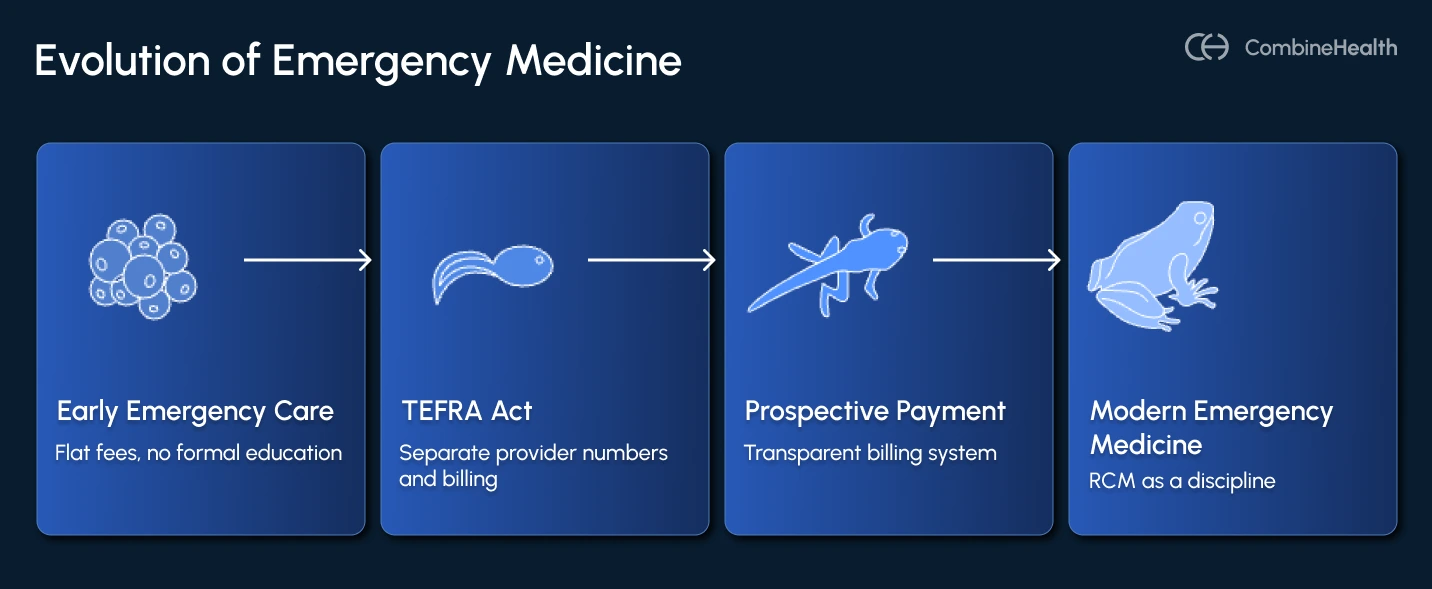
With TEFRA and later the prospective payment system for inpatient hospitals, billing became more transparent—but also more complex. Documentation evolved from a few sentences to several pages.
That’s when revenue cycle management (RCM) emerged as a discipline, and coding, compliance, and documentation became mandatory survival tools for hospitals to get paid.
Core Challenges of the Emergency Department Billing
Fast-forward to today, and the complexity of emergency department coding and billing has multiplied exponentially.
Emergency departments that once relied on handwritten notes and brief summaries now produce 20-page charts packed with:
- Detailed clinical narratives
- Diagnostic justifications
- Payer-mandated documentation requirements
While this documentation reflects progress, it has also introduced new challenges. Despite better data and digital systems, claim denials continue to rise, and Caral believes the system is approaching a breaking point.
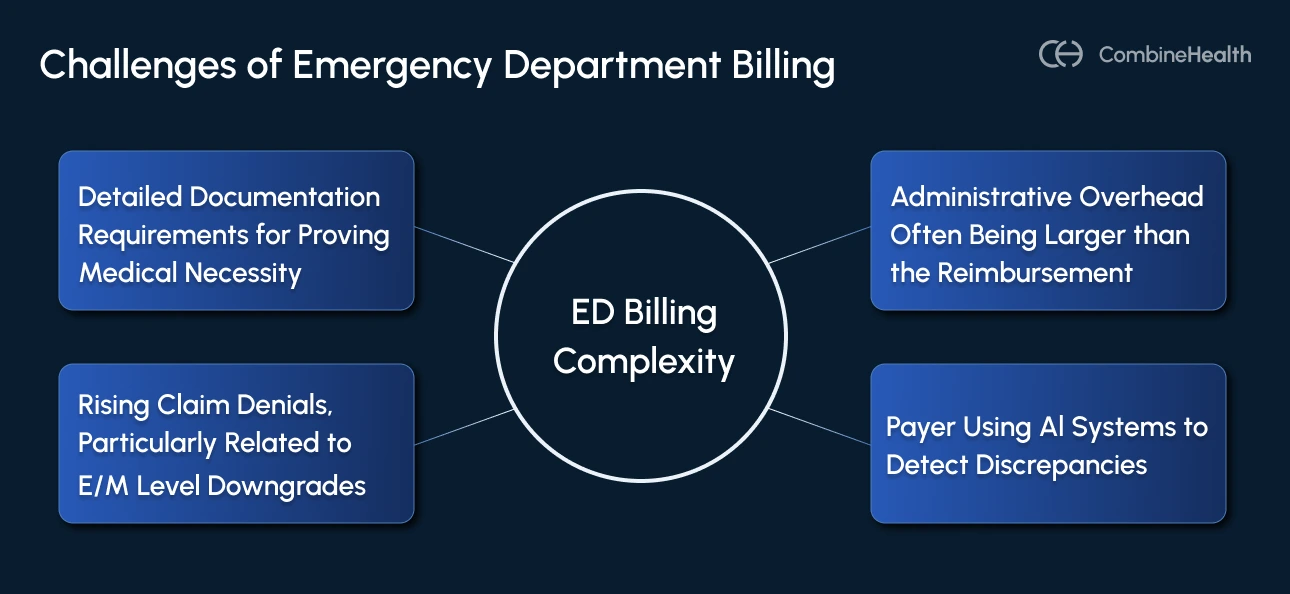
Think about the cost of just one denied claim.
If a Level 5 E/M visit is downgraded to a Level 4, the difference in payment might seem small in isolation—but multiplied across thousands of visits, the impact is enormous.
Even when a claim is successfully appealed, the reimbursement gained rarely offsets the administrative overhead—the hours of compliance review, legal input, and staff time required to fight it. Multiply that across an ED that handles tens of thousands of visits a year, and the losses can be staggering.
.webp)
On Payers Using AI
A major reason behind this strain is that payers have evolved, too. They’ve built their own sophisticated ecosystems of algorithms and automation that:
- Track medical billing and coding patterns across providers
- Redefine what counts as medical necessity
- Use AI to detect discrepancies or outliers before payment
This has created a new kind of administrative burden for emergency departments. What used to be a shared clerical responsibility is now handled by entire departments dedicated to denial management, legal claim appeals, and compliance audits.
Challenges with AI Adoption in the Emergency Department
When asked what challenges she’s seen as AI enters the emergency medicine workflow, Caral states that its success depends on how thoughtfully it’s implemented and understood by the people using it.
For this, she follows two approaches:
1. Reassuring Staff And Making Them AI-Ready
Caral believes that AI succeeds when it complements (not competes with) human expertise. Instead, she follows an administrative simplification approach, where she trains her team to focus on consistency of AI results.
The goal is to ensure the work AI performs is done accurately and reliably, identifying and eliminating process glitches before they escalate.
2. Understanding Client Needs Before Implementation
The second priority, she says, is understanding each client’s unique needs—and why those needs exist.
In medical coding, accuracy thresholds are everything. Most contracts expect a 95–97% accuracy rate, but the level of complexity in emergency department charts can make that challenging.
Each E/M code represents a complex intersection of data points—from history and physical findings to decision-making and clinical documentation. The more complex the case, the more opportunities there are for errors or interpretation gaps.
Caral explains that her team evaluates clients based on variables such as:
- Specialty focus (pediatrics, trauma, rural medicine, etc.)
- Facility type (urban vs. rural, community vs. teaching hospital)
- Resource constraints (staffing, technology, payer mix)
How RCM Teams Can Responsibly Use AI in the Emergency Department Billing
Today’s technology can slice and dice every statement, every code, and every billable event in extraordinary detail. AI can provide granular visibility—daily, weekly, monthly, even provider-level analytics—to support performance tracking and compliance improvement.
However, Caral cautions that more data doesn’t always mean better outcomes.
.webp)
Automation has replaced manual calculations and recordkeeping, but the human element remains critical. Even with advanced systems, ED billing success still depends on:
- Accurate source documentation
- Proper data structure and capture
- Continuous auditing and feedback loops
- Adaptability to each practice’s unique workflows
Using AI for Enhancing ED Billing Accuracy
Modern AI tools have made it possible to achieve a level of accuracy once unimaginable with handwritten charts.
Caral points out that AI’s success is only as strong as the data it’s trained on. It can automate calculations, apply payer logic, and identify anomalies. But, it must still be taught how to interpret what’s clinically important versus what’s just digitally available.
A one-size-fits-all AI model won’t work; what’s needed is customized AI that learns each practice’s workflow and builds accuracy over time.
That’s where Sourabh Agrawal, CEO of CombineHealth, offers some perspective.
Sourabh explains that every coding process has two distinct components:
- The creative side: interpreting guidelines, applying judgment, and understanding medical necessity.
- The repetitive side: assigning standardized codes and reviewing similar chart types repeatedly.
Key Takeaways for Emergency Department RCM Teams
The story of emergency medicine’s evolution is ultimately about adaptation. Every shift, from TEFRA to modern payer algorithms, has demanded that RCM teams grow smarter, not just faster.
For today’s emergency departments, the lesson is clear: the work is about building resilient, data-aware systems that can sustain financial health without losing sight of the people behind them.
- Don’t just chase automation, design for consistency
- Measure AI accuracy, not activity
- Train AI like you train junior staff
- Recognize that payer AI is evolving, too
- Keep human review central to all RCM workflows
At CombineHealth, we’re helping emergency departments put these principles into action. Our AI workforce (AI agents like Amy, the medical coder, and Marc, the medical biller) works alongside human teams to simplify complex workflows, reduce denials, and accelerate collections without compromising compliance.
Schedule a demo to know more!
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai






.webp)









