Automated Insurance Verification: Why Hospitals Should Move On From Manual Methods
Manual insurance verification leads to errors, denials, and delays. Learn how automated insurance verification improves accuracy, efficiency, and patient trust.
January 20, 2026
.webp)

Key Takeaways:
• Manual insurance verification is inconsistent, time-intensive, and prone to preventable errors.
• Eligibility-related denials are among the most common and avoidable sources of revenue leakage.
• Automated insurance verification ensures every patient is verified the same way, every time.
• Early verification improves patient transparency and reduces billing disputes.
• Automation shifts insurance verification from a reactive task to a proactive control point
• The biggest impact comes from automating workflows, not just eligibility checks.
• Human oversight remains essential, with automation handling repetitive verification work.
• Moving beyond manual methods is no longer optional for predictable revenue and patient trust.
Insurance verification looks simple on paper. Check eligibility. Confirm benefits. Move the patient forward.
In reality, it’s one of the most fragile points in the healthcare revenue cycle.
An AMA survey shows that practices spend approximately 13 hours just on prior authorization paperwork and phone calls. When you add manual eligibility checks on top of that, it’s clear that payer-facing admin work is one of the largest hidden drains in healthcare.
Manual insurance verification creates delays, inconsistencies, and downstream denials, yet many hospitals still rely on it simply because ‘that’s how it’s always been done.’
Automated insurance verification changes this entirely. It removes guesswork, reduces human error, and gives revenue cycle teams real-time clarity before a patient ever walks in the door.
This article breaks down what manual insurance verification gets wrong, how automated insurance verification works in modern healthcare systems, and why hospitals can no longer afford to treat it as an afterthought.
What Is Automated Insurance Verification?
Automated insurance verification is the use of AI-driven workflows to confirm a patient’s insurance eligibility, network status, benefits, and financial responsibility without relying on manual staff intervention.
Instead of staff logging into multiple payer portals, copying data into spreadsheets, and interpreting plan rules by hand, automated insurance eligibility verification systems do this work programmatically—using payer integrations, rules engines, and real-time data retrieval.
At a high level, automated insurance verification helps healthcare teams:
- Confirm whether a patient’s insurance is active
- Determine in-network vs out-of-network status
- Extract benefit details like copays and deductibles
- Identify pre-authorization requirements
- Estimate patient financial responsibility before the visit
For medical coders, billers, and denial managers, this means fewer surprises after services are rendered and fewer avoidable claim denials downstream.
How Manual Insurance Verification Works Today (And Where It Breaks)
Most healthcare organizations still rely on manual insurance verification to confirm patient eligibility and benefits before a visit. While workflows may vary by practice size or specialty, the core process and its weaknesses remain the same.
Manual insurance verification is often treated as a routine front-desk task.
Typical Manual Insurance Verification Workflow
A standard manual process usually looks like this:
- Front-desk or billing staff collect insurance details during scheduling or check-in.
- Staff log into one or more payer portals, often using separate credentials.
- They manually search for the patient’s policy using member IDs and demographics.
- Network status is checked—sometimes only at the plan level, not the provider level.
- Benefits such as copays, deductibles, and coverage limitations are reviewed and interpreted.
- Notes or screenshots are entered into the EHR or practice management system.
On the surface, this process appears straightforward. In reality, it sits at the intersection of patient experience, billing accuracy, and denial prevention. When it breaks down, the impact ripples across the entire revenue cycle.
Key Limitations of Manual Insurance Verification
Every step in manual insurance verification depends heavily on human accuracy, availability, and judgment. Any delay, distraction, or misunderstanding can introduce errors that surface much later, even after services are rendered.
Here’s where manual insurance verification falls short:
Time-intensive and repetitive work
Eligibility checks can take anywhere from a few minutes to much longer per patient, especially when payer portals are slow, unresponsive, or require multiple logins. Multiply this by dozens or hundreds of patients per day, and verification quickly becomes a bottleneck.
High error rates
Small mistakes, like entering an incorrect policy number, overlooking a coverage exclusion, or relying on outdated eligibility information, can lead directly to claim rejections and downstream denials.
Inconsistent verification standards
Manual workflows vary by staff member and workload. Some verify network status thoroughly. Others focus only on eligibility. Benefits may be reviewed in detail or skipped entirely when time is tight.
Limited documentation and audit trails
Manual notes rarely include payer-specific language, timestamps, or supporting evidence. When claims are denied, teams often lack the clinical documentation needed to support appeals.
Delayed patient communication
When eligibility or coverage issues surface after the visit, patients feel blindsided. Bills trigger confusion, frustration, and disputes, damaging trust and slowing collections.
Taken together, these gaps explain why eligibility-related denials remain one of the most common and most preventable sources of revenue leakage in healthcare today.
Eligibility-Related Denials: Why They Happen So Often
Eligibility-related denials rarely stem from clinical issues. They’re usually the result of breakdowns at the front end of the revenue cycle, during insurance verification and registration.
Common causes include:
- Coverage that is inactive or has changed since scheduling
- Services rendered out of network due to incomplete network checks
- Incorrect or outdated patient insurance information
- Missed or misunderstood benefit limitations
- Authorization requirements identified too late
In manual workflows, these issues are easy to miss. Eligibility is often verified once, under time pressure, and without rechecking closer to the visit. Payer portals may return incomplete or hard-to-interpret information, leaving staff to rely on judgment rather than consistent rules.
As a result, eligibility issues surface only after the claim is submitted, requiring rework, appeals, or write-offs.
Automated eligibility verification helps prevent these denials by verifying coverage consistently, applying payer-specific rules, and flagging issues before care is delivered. By catching eligibility, network, and authorization risks early, automation turns one of the most common denial categories into one of the most preventable.
How Automated Insurance Verification Works in Healthcare Systems
Automated insurance verification replaces manual checks with system-driven workflows that run in the background of patient intake and scheduling.
Instead of staff logging into multiple payer portals, automation verifies insurance as soon as patient information is captured.
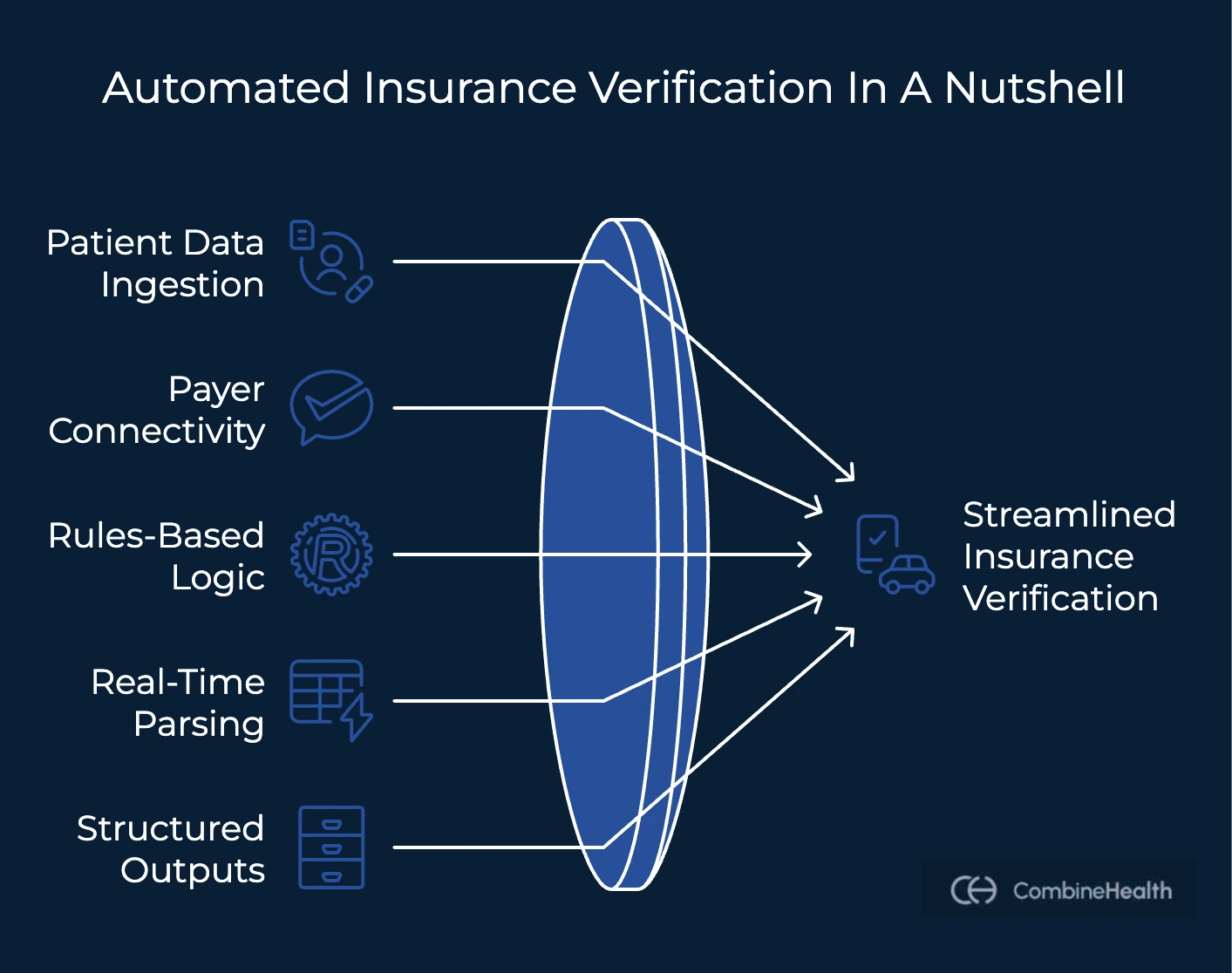
Core Components of Automated Insurance Verification
Most modern automated insurance verification healthcare systems are built around a few essential components:
- Patient data ingestion from scheduling or intake systems: Insurance details are pulled automatically from appointment scheduling, pre-registration, or digital intake forms. No manual re-entry is required.
- Direct connectivity to payer portals and clearinghouses: The system connects directly to payer portals and clearinghouses to retrieve eligibility and coverage data in real time.
- Rules-based eligibility and benefit logic: Payer responses are interpreted using predefined rules. This removes guesswork and reduces variation across staff members.
- Real-time response parsing and documentation: Eligibility results are parsed instantly and documented in a consistent, auditable format.
- Structured outputs for downstream workflows: Verified eligibility and benefit details flow directly into billing and coding systems, supporting cleaner claims and faster follow-up.
The result is faster, more consistent verification. Automated systems flag inactive coverage, out-of-network plans, and authorization needs before the visit, giving teams time to act. Embedded into intake workflows, automation turns verification into a proactive control point that reduces denials and improves patient communication.
How CombineHealth Automates Insurance Verification with Mark
Within CombineHealth’s platform, insurance verification is handled end-to-end by Mark, CombineHealth’s AI Medical Billing Solution.
As soon as patient intake data is received, Mark automatically initiates insurance verification, without waiting for front-desk or billing staff to intervene. Mark owns the full insurance verification workflow, ensuring every patient is verified consistently before care is delivered.
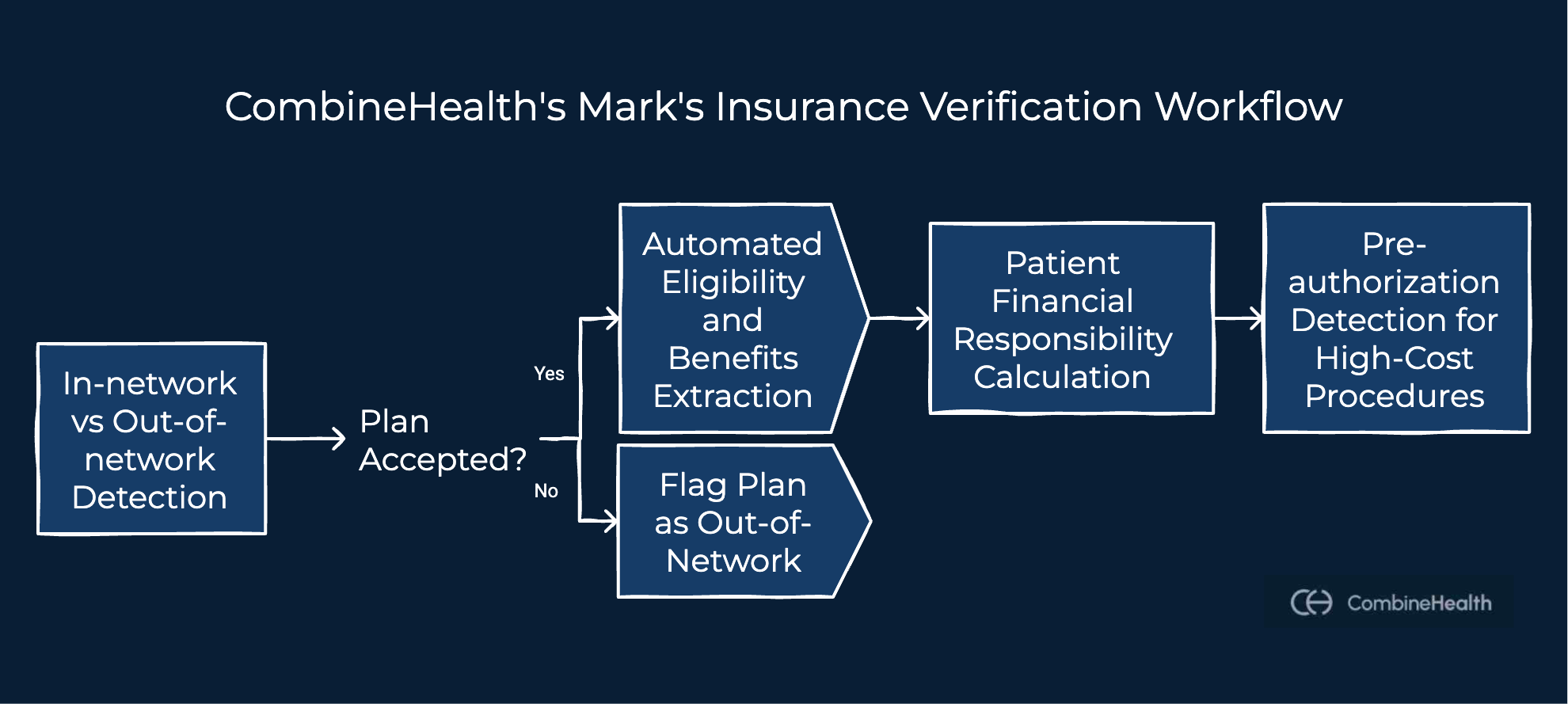
Specifically, Mark handles four critical verification workflows:
- In-network vs out-of-network detection: Mark confirms whether the patient’s plan is accepted at the clinic or provider level. If a plan is out of network, it is flagged immediately so the patient can be informed before the visit.
- Automated eligibility and benefits extraction: Once network status is confirmed, Mark retrieves benefit details such as copays, deductibles, coinsurance, and coverage limits by connecting directly to payer portals like Availity and TriZetto.
- Patient financial responsibility calculation: For each appointment type, Mark uses predictable CPT codes to estimate expected patient costs based on deductible and copay rules. These estimates can be surfaced before the visit to improve transparency and collections.
- Pre-authorization detection for high-cost procedures: Mark identifies visits that may require prior authorization based on procedure type, payer-specific rules, and coverage thresholds, reducing preventable denials later in the revenue cycle.
All verification results are structured, explainable, and designed to support human review. This keeps staff in control while eliminating repetitive verification work.
.webp)
Benefits of Automation in Insurance Verification for Healthcare Providers
The benefits of automation in insurance verification in healthcare extend far beyond faster eligibility checks. Automation improves how information flows across the entire revenue cycle—before claims are submitted, before patients are seen, and before denials occur.
With automation, eligibility and benefit checks are performed the same way for every patient. This consistency reduces missed network issues, overlooked coverage limitations, and incomplete documentation, three common causes of avoidable denials.
For front-desk and billing teams, automation removes repetitive portal logins and manual data entry. Automation also shifts insurance verification from a reactive task to a proactive control point. Coverage issues, out-of-network plans, and authorization requirements are identified before care is delivered, giving teams time to notify patients or adjust next steps.
For medical coders, billers, and denial managers, the impact is immediate. Cleaner eligibility inputs lead to cleaner claims. Fewer surprises lead to fewer rework cycles. And better documentation strengthens the denial appeal process when denials do occur.
In short, automated insurance verification doesn’t just speed up workflows but also stabilizes revenue and improves patient trust at the front end of the care journey.
Best Practices for Automating Insurance Verification for Patients
To get full value from automated insurance verification, healthcare organizations must embed it early and apply it consistently.
- Start verification at patient intake, not at check-in, so coverage issues surface before care is delivered.
- Re-verify eligibility before every visit, since payer status and benefits can change at any time.
- Automate benefit extraction, not just eligibility checks, to capture copays, deductibles, and coverage limits accurately.
- Flag pre-authorization requirements as early as possible to prevent avoidable denials.
- Most importantly, combine automation with human oversight. Automation should handle repetitive verification tasks, while staff review exceptions and make informed decisions.
Automation works best when it supports clinical and billing teams, not when it replaces judgment.
Common Myths About Automating Health Insurance Verification
- “Automation replaces billing staff.”
Automation removes repetitive work, not expertise. Humans still review, approve, and escalate decisions.
- “Manual checks are more accurate.”
Manual checks vary by staff member and time pressure. Automation applies rules consistently.
- “Automation is only for large hospitals.”
Mid-sized clinics often see faster ROI because staffing constraints are more acute.
- “Payer portals already solve this.”
Payer portals provide data, but they don’t standardize workflows or prevent missed steps.
Ready to Move on to Automated Insurance Verification?
Automated insurance verification brings consistency to eligibility, benefits, and authorization checks before care is delivered. CombineHealth helps teams make this shift by embedding AI-driven verification directly into intake and billing workflows, while keeping humans in control.
If reducing denials, improving patient transparency, and easing staff workload are priorities, it may be time to move beyond manual methods. To explore how Mark can help with insurance verification, you can book a demo with us.
FAQs
1. What is automated patient insurance verification in a medical clinic setup?
It’s the use of software-driven workflows to verify eligibility, benefits, and financial responsibility without manual effort.
2. How accurate is automated insurance eligibility verification?
Accuracy improves because rules are applied consistently and payer data is retrieved directly.
3. Does automation work across multiple payer portals?
Yes. Automated systems connect to multiple portals and normalize responses.
4. Can automation detect pre-authorization requirements?
Yes. Automation flags authorization needs based on payer-specific rules.
5. How does automated insurance verification reduce denials?
By catching eligibility, network, and authorization issues before claims are submitted.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai

















