Automated Insurance Claims in Healthcare: How AI Reduces Claims Processing Time
A practical guide to automated insurance claims processing in healthcare—what it is, how it works, and where AI delivers measurable RCM impact.
January 28, 2026


Key Takeaways:
• Manual claims processing is no longer sustainable at scale. Rising claim volumes, payer complexity, and denial rates are pushing traditional RCM workflows past their limits.
• AI-driven claims automation absorbs rule-based work across the lifecycle.
• Automation significantly improves speed, accuracy, and capacity.
• Denial reduction and predictive intelligence drive real revenue impact. By identifying denial risk before submission and prioritizing high-value claims, AI helps reduce rework and improve first-pass yield.
• Successful AI adoption requires a phased, operational approach. Organizations that start with targeted pilots, clear metrics, and strong change management see more durable, system-wide RCM gains.
Automated insurance claims are often talked about as a future-state capability—something complex, risky, or only viable at massive scale. In reality, claims processing has already reached a breaking point where manual workflows can no longer keep up with volume, complexity, or payer variability.
In 2023 alone, U.S. providers spent an estimated $25.7 billion just fighting claim denials—about $57.23 in administrative cost per denied claim. That spend reflects not just lost revenue, but the cumulative weight of rework, follow-ups, appeals, and staff time consumed by preventable friction in the claims process.
That’s where automated insurance claims processing enters as a way to absorb the rule-based, error-prone work that slows claims down and drains resources.
In this guide, we break down what automated insurance claims processing looks like in healthcare today and how it differs from traditional workflows. We also explore which stages of the claims lifecycle can be automated and how organizations can implement AI-driven claims processing to deliver measurable, sustainable impact across the revenue cycle.
What Is Automated Insurance Claims Processing in Healthcare?
Automated insurance claims processing is the end-to-end, technology-driven workflow through which healthcare providers submit claims to insurance companies for reimbursement of services delivered.
In practice, it refers to the application of advanced technologies, such as:
- Artificial Intelligence (AI): Combines ML with rules engines to make context-aware decisions, perform fraud detection, auto-adjudicate claims, and intelligently route complex cases for human review
- Machine Learning (ML): Algorithms learn patterns from historical claims data to predict denial risk, identify fraud indicators, optimize routing decisions, and improve accuracy over time
- LLM: Foundation models trained on vast amounts of medical, billing, and regulatory text to understand and generate human-like language.
- Agentic AI: Autonomous, goal-oriented AI systems that can plan, execute, and iterate across multiple steps in the claims lifecycle.
- Natural Language Processing (NLP): Parses unstructured clinical text to identify and extract medical entities directly from physician notes, imaging reports, and authorization letters
Instead of relying on manual data entry, disconnected systems, and constant human intervention, automation standardizes how claims move through the revenue cycle.
Steps Involved in Traditional Claims Processing
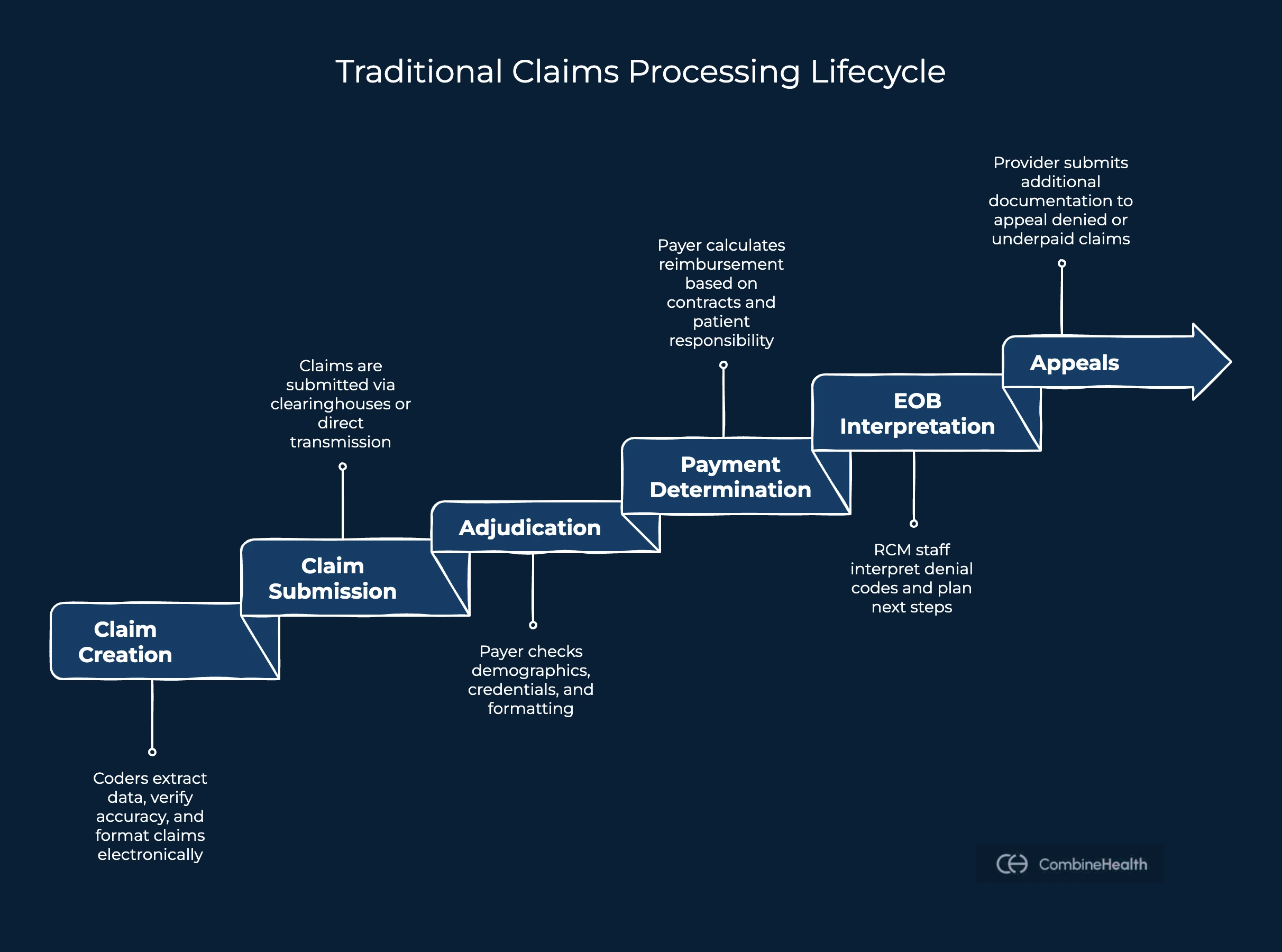
Traditional claims processing follows a six-step lifecycle designed decades ago when paper dominated healthcare:
1. Claim creation: Medical coders extract information from provider documentation, verify coding accuracy against payer-specific rules, and compile claims. This information is compiled into standardized electronic forms (CMS-1500 for professional claims, UB-04 for institutional claims) or ANSI 837 data files.
2. Claim submission: Claims are submitted to insurance payers through electronic clearinghouses or direct transmission. RCM staff manage submission schedules, track confirmation receipts, monitor which payers have received claims, and follow up if acknowledgments are delayed.
3. Adjudication: The payer performs basic validation: verifying patient demographics (name, DOB, insurance ID), provider credentials, service dates, and basic claim formatting. Missing or incorrect information triggers instant rejection, sending the claim back to the provider for correction.
4. Payment Determination: After passing all review stages, the payer calculates the reimbursement amount based on contracted fee schedules, applies deductibles and copayments, and determines patient responsibility.
5. Explanation of Benefits (EOB) Interpretation: The payer creates an EOB detailing what was approved, what was denied, and the denial reasons (if applicable). The RCM staff interpret denial codes, map them to clinical or documentation gaps, and decide on next steps.
6. Appeals: When a claim is denied or underpaid, providers initiate claim appeals by submitting additional documentation, clinical evidence, or policy clarifications to challenge the payer's decision. The process involves analyzing the denial reason, researching payer policy, gathering clinical documentation evidence, preparing appeal letters, tracking appeals status, and so on.
Manual vs. Automated Claims Processing: What Actually Changes?
The shift from manual to automated claims processing doesn’t create incremental improvement—it fundamentally changes how claims move through the revenue cycle.
Below is a quantified comparison across these operational metrics that define claims performance at scale:
1. Processing Speed
Industry data estimates an overall claims processing and payment window of 4–6 weeks in largely manual environments. This figure reflects full cycle time, including submission, payer review, back-and-forth communication, and payment.
Automated claims processing compresses this cycle significantly.
Research shows that intelligent automation can reduce total claims processing time by up to 50% compared with manual workflows, significantly compressing cycle time and accelerating reimbursement while also improving accuracy and fraud detection.
2. Claim Volume Capacity
A single billing staff member can possibly process about 10–15 claims per hour in manual workflows. But, automated systems process 150+ claims within minutes (CombineHealth’s Findings).
For organizations handling 500–1,000 claims daily, automation removes the need to scale staffing linearly as volume grows.
3. Error Reduction
Manual claims processing is inherently error-prone. Human reviewers must juggle changing payer rules, modifiers, documentation requirements, and time pressure—creating predictable failure points across coding and submission.
AI systems (when implemented well) can offer a claims processing accuracy of up to 97% (CombineHealth’s proven statistic). The shift from retrospective correction to pre-submission validation makes this possible.
4. Denial Rate Improvement
Industry-wide initial denial rates now average roughly 12%, up from 9.6% in 2022. AI solutions like CombineHealth have managed a 20% reduction in denials for a very high volume of claims (10,000+ claims).
.webp)
5. Cost To Collect
Cost to collect is a core revenue cycle metric that measures how much a healthcare organization spends to collect every dollar of patient revenue.
It’s one of the clearest indicators of RCM efficiency because it captures both:
- Operational complexity (manual work, rework, denials)
- Labor intensity (how many human touches are required)
McKinsey’s analysis suggests that a largely AI-driven, ‘touchless’ revenue cycle could cut cost-to-collect significantly. For a health system with $6 billion in patient revenue, even a modest 1–2 percentage-point reduction equates to $60 million to $120 million in savings annually.
What Stages of the Claims Lifecycle can be Automated?
As per research, about 50–70% of the claims lifecycle is routine, rule-based, and highly automatable.
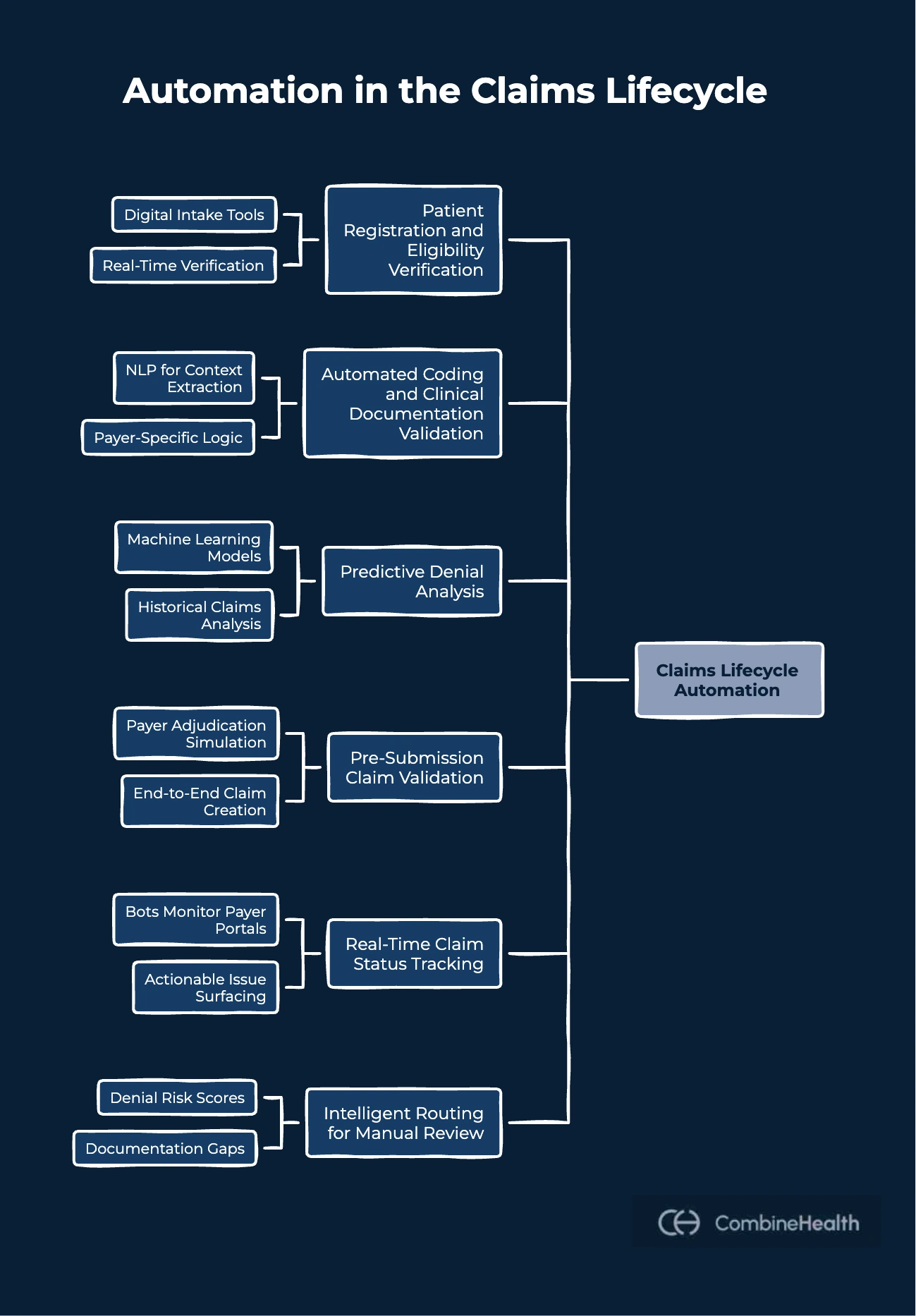
Below is a breakdown of where automation applies across the major stages of the claims lifecycle:
Patient Registration and Eligibility Verification
Automation begins before a claim is ever created. Digital intake tools access self-service portals or kiosks to capture details like:
- Patient demographics
- Insurance details
- Visit information
Additionally, eligibility and coverage are verified in real time against payer systems, identifying inactive coverage, coordination-of-benefits issues, and prior authorization requirements upfront.
For instance, CombineHealth’s Mark (AI Medical Billing Solution) integrates eligibility verification and payer rule checks early in the workflow, preventing claims from entering the system with invalid or incomplete data.
Automated Coding and Clinical Documentation Validation
AI extracts clinical context from provider notes using NLP, assigns ICD-10 and CPT codes, and validates that documentation supports coded services.
CombineHealth’s Amy (AI Medical Coding Solution) is designed for this exact workflow. The AI agent:
- Reads encounter notes directly from the EHR
- Applies payer-specific coding logic
- Provides line-by-line rationale for every coding decision
Predictive Denial Analysis
Machine learning models analyze historical claims, payer behavior, diagnosis-procedure combinations, and documentation completeness to identify claims likely to be denied before submission.
In this scenario, CombineHealth’s Adam (AI A/R Followup Solution) incorporates priority rules (by age, dollar value, payer, etc.), so that high-yield claims are worked first.
Pre-submission Claim Validation
Before claims are transmitted, automated systems simulate payer adjudication by applying coverage rules, medical necessity checks, authorization validation, and formatting requirements.
CombineHealth’s Mark applies payor-specific billing SOPs and validates codes and modifiers while preparing charges for claim submission. The AI agent also handles claim creation end-to-end and works across EHR and billing systems.
Real-time Claim Status Tracking
Instead of manual status checks that can take hours, bots monitor payer portals continuously and surface only actionable issues.
For instance, CombineHealth’s Adam navigates payer portals, chatbots, and IVRs autonomously, freeing staff from status hunting.
Intelligent Routing for Manual Review
High-value or policy-sensitive claims are routed to human reviewers with pre-analyzed context—denial risk scores, documentation gaps, and policy excerpts.
A good AI solution is the one that ensures humans intervene only where judgment is required, not where rules suffice.
Automated Denial Analysis and Appeal Prioritization
AI determines whether denials are appealable, identifies supporting clinical documentation, and prioritizes cases by revenue impact. Then, AI also helps in generating appeal letters using clinical evidence and payer policy citations, then submitted automatically with follow-up tracking.
For example, Rachel, CombineHealth’s AI Appeals Assistant, drafts payer-specific appeal letters backed by coding rationale and policy evidence.
How to Implement AI in Claims Processing Workflows
Implementing AI in claims processing is an operational transformation. That’s why most healthcare organizations follow a phased implementation approach, progressing from controlled pilots to scaled, system-wide automation.
Phase 1: Assessment and Planning
Begin by mapping existing claims workflows end to end—from patient intake through payment posting. The objective is to surface friction points and quantify baseline performance across key metrics:
- Denial rate
- Cost per claim
- Cost to collect
- Processing time
- A/R days
- Staffing effort and rework patterns
Then, evaluate completeness, consistency, and standardization across claims, clinical documentation, and payer data.
Meanwhile, assess your existing technology stack, including EHRs, billing platforms, clearinghouses, and payer connections. Notice if the following bottlenecks exist:
- Integration points and API readiness
- Legacy system constraints
- Manual handoffs between systems
Phase 2: Vendor Selection and RFP Process
Issue an RFP that clearly defines success criteria, including:
- Scope of automation (which claims stages?)
- Accuracy standards (95%+ minimum)
- Explainability and auditability
- Compliance requirements (HIPAA, state regulations)
- Implementation timeline
- Pricing model (SaaS, per-claim, or hybrid)
Phase 3: Pilot Deployment
Deploy AI on a limited slice of claims, typically a single specialty, payer, or 5–10% of total volume. AI outputs should be audited against manual review to confirm performance meets or exceeds benchmarks.
Key validation metrics include:
- First-pass accuracy
- Precision (true positives among flagged claims)
- Recall (issues correctly identified)
- Processing time per claim
- Exception rate (claims requiring human review)
Phase 4: Staff Training and Change Management
Train billing, coding, and RCM teams on new workflows, dashboards, and escalation paths. Make sure to establish clear communication protocols and feedback loops early to capture workflow friction and adoption issues.
Phase 5: Scaled Rollout
AI models must be retrained monthly or quarterly to account for new payer policies, updated procedure codes, and evolving care patterns.
Turn Claims Automation Into Measurable RCM Impact
The real challenge with claims automation isn’t whether it works—it’s knowing where to start, what to automate, and how to do it without disrupting what already works. And for organizations that have already invested in automation or AI, the question often becomes whether those tools are truly reducing friction—or simply shifting it elsewhere in the workflow.
If you’re already seeing pressure from denials, staffing constraints, or longer reimbursement cycles, it may be worth taking a closer look at how your current claims processes are supported today.
Case Study: CombineHealth Cuts Eligibility Verification Time by 80% for an Anesthesia Group
A short demo with CombineHealth can help clarify that. We’ll walk through how our AI fits into your existing claims workflows, where bottlenecks typically emerge, and how teams use CombineHealth to improve accuracy and throughput without adding operational complexity.
Book a demo today!
FAQs
Can AI be used in claims processing?
Yes. AI is widely used in claims processing to automate medical coding, validation, submission, status tracking, and denial analysis. It handles routine, rule-based tasks while routing complex or ambiguous cases to human experts for review.
Are insurance companies using AI to deny claims?
Insurers use AI to review claims for eligibility, coverage rules, and potential fraud, but denials are still governed by payer policies. In practice, AI is used to flag issues, not make unilateral denial decisions without human oversight.
How much time can AI and RPA save on claims processing?
AI and RPA can reduce claims processing time by 30–70%, depending on workflow maturity. Routine claims that once took days or weeks to move through the system can often be processed within hours when automation is applied effectively.
What technologies are typically used to automate claims?
Claims automation typically uses a combination of AI, machine learning, robotic process automation (RPA), LLMs, agentic AI, and natural language processing (NLP), integrated with EHRs, billing systems, and payer portals.
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai





.webp)










