The Building Blocks of a Financially Resilient Health System
Explore the key components of a financially resilient and profitable health system and how these components go hand in hand.
January 23, 2026


Financial resilience in today’s clinics and health systems doesn’t come from working harder or hiring more staff. It comes from controlling the few levers that actually determine whether care turns into cash.
There are only two that truly matter:
- Good patient intake
- Good revenue cycle management
Everything else (denials, delayed payments, rising A/R, and margin pressure) is a downstream consequence of how well these two functions work together.
In this article, we’ll break down why patient intake and revenue cycle management are crucial pillars of a healthcare organization’s financial system—and how to go about strengthening them both.
Let’s explore them one by one, starting where the revenue cycle actually begins.
Patient Intake: What Is It and Why Does It Matter?
Patient intake is the structured process of collecting, verifying, and recording a patient’s demographic, clinical, and insurance information before care is delivered. It sets the foundation for both clinical decision-making and downstream billing and reimbursement.
According to a CGS Medicare 2025 Top Denials Report, one of the top claim denial reasons was “Services Not Covered by a Contractor,” as it requires patient eligibility/registration verification.
Patient intake is where the revenue cycle either succeeds or fails.
This finding represents a fundamental shift in how healthcare leaders should think about registration as a critical control point, and not just a clerical function.
After all, a claim is only as strong as the data that built it. When patient information is captured poorly, insurance eligibility is never verified, and clinical documentation doesn't justify the services rendered, claims become fragile.
The Traditional Patient Intake Workflow and Where It Lacks
For many health systems, patient intake still looks much the same as it did years ago—paper-heavy, manual, and reactive.
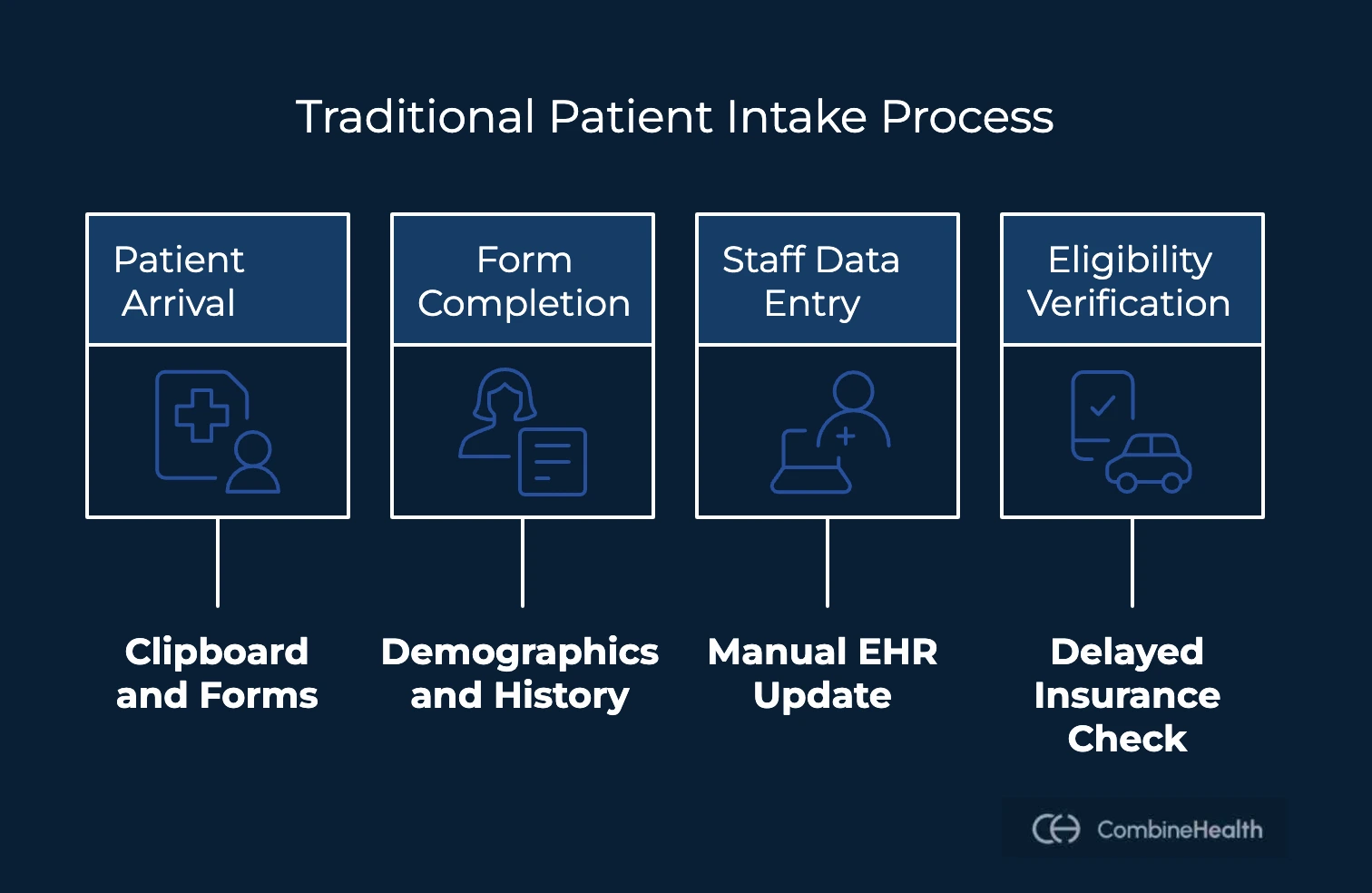
Here’s what the process traditionally looks like:
- A patient arrives and is handed a clipboard with paper forms.
- These forms collect demographics, insurance information, medical history, and consent.
- After the visit (or sometimes during it), front-desk staff manually enter this information into the EHR or practice management system.
- Insurance eligibility is verified later (often via phone calls or payer portals), sometimes only after the visit has already occurred.
While familiar, this workflow quietly introduces financial and operational risk at the very first touchpoint. Here’s how:
- Manual transcription drives errors from illegible handwriting, typos, and missed fields.
- Insurance verification is delayed, so coverage issues surface only after claims are submitted.
- Duplicate or inconsistent patient records are created when names or details are entered differently.
- Staff time is consumed by data entry instead of patient-facing work, and patients endure longer waits and redundant paperwork.
And the hidden cost of doing things “the way it’s always been done”?
The damage doesn’t show up immediately. The visit still happens. The claim still gets submitted. But the intake data underneath it is weak—setting the stage for denials, delays, and avoidable rework later in the revenue cycle under payer scrutiny.
Common Claim Denials Due to Patient Registration Errors
When patient and insurance information is incomplete, outdated, or incorrect at intake, payers often reject the claim outright before medical necessity or coding is even considered.
These are some of the most frequent (and preventable) intake-related breakdowns:
- Name or date of birth mismatches: If patient identifiers don’t exactly match payer records, the claim can’t be matched to a member and is rejected immediately.
- Outdated or incorrect insurance plans: Patients change jobs, employers switch carriers, or plans renew annually. When systems aren’t updated in real time, clinics bill the wrong payer or plan.
- Missing policy details: Absent policy numbers, group numbers, or secondary insurance information leave claims incomplete and vulnerable to rejection.
- Eligibility verification errors: Without checking eligibility before or during the visit, inactive coverage is often discovered only after the claim is submitted—and denied.
- Prior authorization gaps: Required prior authorizations that are not obtained, expired, or improperly documented on the claim almost guarantee a denial, regardless of clinical validity.
Digital Patient Intake: How It Solves the Limitations of the Traditional Approach
The biggest shift with digital patient intake is control. By moving data capture upstream and validating it automatically, digital intake turns registration from a manual task into a revenue-protecting system.
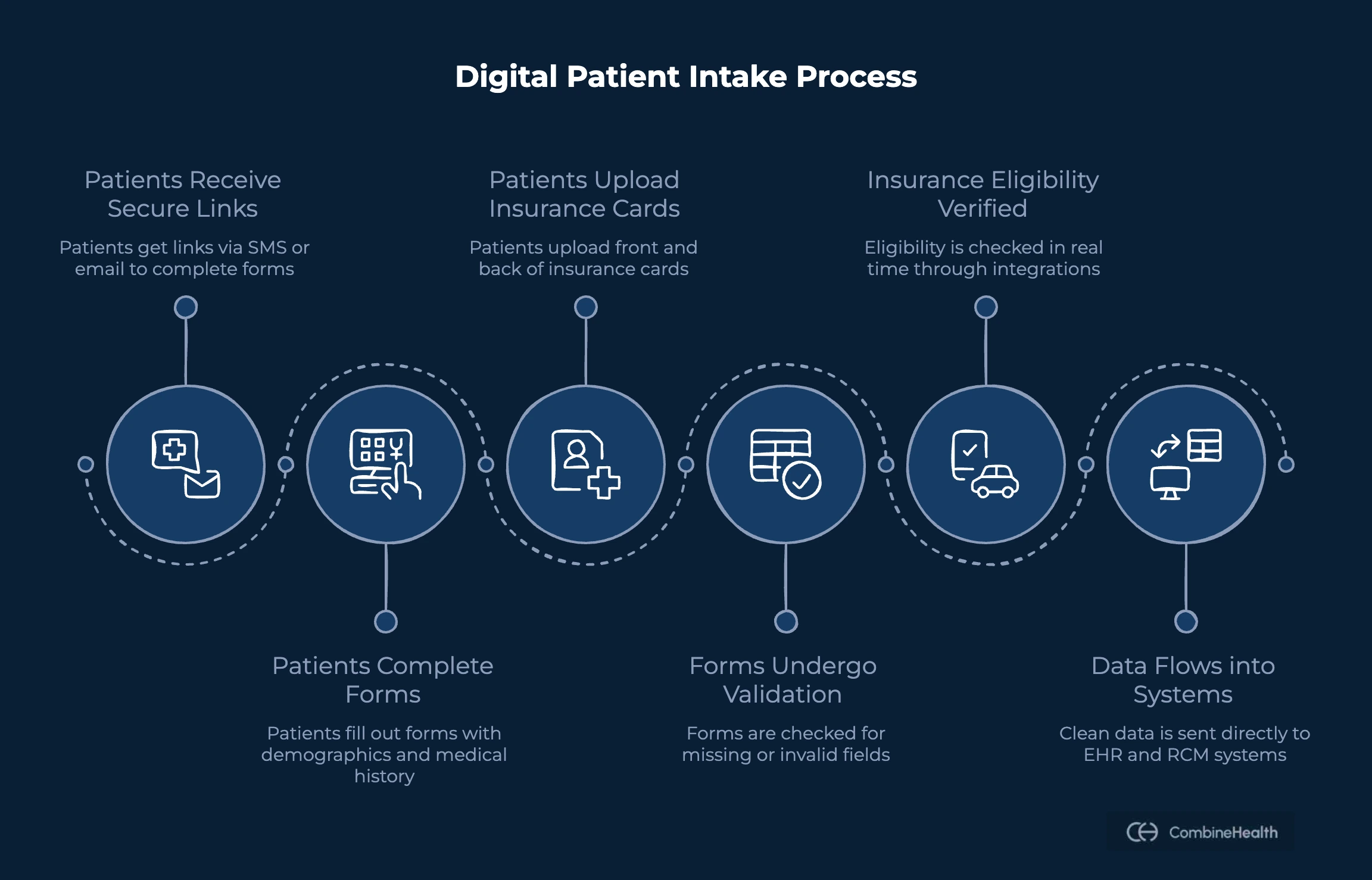
Here’s how the process typically works:
- Patients receive secure links via SMS or email to complete intake forms before their visit.
- Forms collect demographics, consent, medical history, and insurance details—including front and back uploads of insurance cards.
- Built-in logic prevents submission if required fields are missing or clearly invalid.
- Insurance eligibility is verified in real time through payer integrations.
- Clean, structured data flows directly into EHR and RCM systems—no manual transcription required.
Why Digital Patient Intake Outperforms Paper-Based Registration Workflows
Compared to traditional intake, digital workflows create measurable operational and financial gains, such as:
- Eliminating handwriting and re-entry significantly reduces typos, mismatches, and incomplete records
- Automating checks and required fields catches issues before the visit
- Improving patient experience by offering the ability to complete forms at home on any device
- Lowering the administrative burden of front-desk teams as they spend less time on data entry and more time handling patient needs
Voice AI for Lead Qualification and Patient Conversion
Patients today discover clinics through paid ads, social media, website chats, and inbound calls, and they expect immediate, personalized responses. When follow-up is delayed or inconsistent, interest fades quickly.
As lead volume grows, clinics face a familiar tradeoff: either add headcount or accept leakage.
Voice AI removes that tradeoff.
Voice AI systems engage, qualify, and nurture patient demand automatically—across channels and around the clock:
- Leads are captured the moment they arrive, not hours later.
- Intent is qualified through natural conversation, not rigid forms.
- Common questions are answered instantly.
- Patients are guided seamlessly toward booking.
For example, Dezy It’s DIVA 360° is built for healthcare organizations managing high lead volumes across ads, social media, websites, and inbound calls. The voice AI platform:
- Captures inbound patient demand 24/7 via calls and web chat
- Qualifies intent, answers questions, and converts leads into booked appointments
- Syncs patient data in real time with leading EHRs and CRMs, ensuring clean, structured records
Revenue Cycle Management: What Is It and Why It Matters?
Revenue Cycle Management (RCM) is the end-to-end process that tracks a patient’s financial journey—from the very first point of contact, such as scheduling or intake, all the way through final payment and account closure.
At its core, RCM connects clinical care with administrative and financial execution. It ensures that services provided are accurately documented, correctly coded, properly billed, and reimbursed on time.
A well-run revenue cycle:
- Reduces preventable denials and write-offs
- Shortens time-to-payment and stabilizes cash flow
- Ensures compliance with payer rules and regulations
- Protects margins amid shrinking reimbursements and rising costs
Steps Involved in Healthcare Revenue Cycle Management
Below is a clear, high-level breakdown of the major phases involved in a typical healthcare revenue cycle:
1. Pre-service: Setting the Financial Foundation
Everything begins before the patient is seen. This phase determines whether the service can be reimbursed at all.
Key activities include:
- Scheduling and patient registration
- Insurance eligibility and benefits verification
- Prior authorization determination and submission
- Patient cost estimates and financial responsibility communication
2. Service: Documenting What Was Delivered
Once care is provided, clinical and financial accuracy must stay aligned.
This phase includes:
- Clinical documentation by providers
- Charge capture for all billable services
- Medical coding based on documentation and guidelines

3. Claims Preparation: Validating Before Submission
Before a claim ever reaches a payer, it must be structurally and logically sound.
Typical steps are:
- Charge entry into the billing system
- Claim scrubbing for errors, missing fields, and rule violations
- Compliance and payer-specific checks
4. Claims Submission and Adjudication: Where Payers Decide
Once claims are sent, payers review them for eligibility, coverage, coding accuracy, and medical necessity.
This phase involves:
- Electronic claim submission
- Payer adjudication
- Claim status tracking and follow-up
5. Payment posting and reconciliation: Making sense of what was paid
After adjudication, payments must be applied correctly to understand what’s still owed.
This includes:
- Posting payments from ERAs and EOBs
- Reconciling allowed amounts versus expected reimbursement
- Identifying underpayments or discrepancies
6. Patient billing and collections: Closing the loop
The final phase focuses on patient responsibility and account resolution.
Key activities:
- Generating and sending patient statements
- Managing follow-ups and payment plans
- Handling write-offs and account closure
Challenges Revenue Cycle Teams Face Today
Even well-staffed billing teams struggle managing revenue cycle if they are not well-equipped and well-prepared. Here are the challenges healthcare organizations encounter most often:
- Claim denials and rejections: Many denials are preventable, yet they continue to consume time and revenue. Some common drivers are:
- Inaccurate or incomplete patient and insurance data
- Missing or expired prior authorizations
- Documentation gaps that fail to support billed services
- Managing long A/R cycles: Unresolved claims, repeated corrections, and delayed submissions stretch accounts receivable timelines. The impact:
- Revenue stays tied up longer than expected
- Cash flow becomes unpredictable
- Finance teams lose visibility into what will actually be collected
- Documentation gaps triggering medical necessity denials: Clinical documentation must do more than reflect care. It must justify reimbursement. But if the documentation misses specificity or is incomplete and completely fails to prove the linkage between diagnosis and procedure, denials are inevitable.
- Coding complexity and constant payer rule changes: Medical coding sits at the intersection of clinical care and reimbursement—and that intersection is constantly shifting. As a result, RCM teams deal with:
- Frequent updates to CPT, ICD-10, and HCPCS codes
- Payer-specific rules that vary by plan and contract
How AI Helps Solve Healthcare RCM Challenges
Healthcare revenue cycles break because the volume, complexity, and variability have outpaced what manual workflows can reliably handle. This is where AI-powered RCM solutions like CombineHealth change the equation.
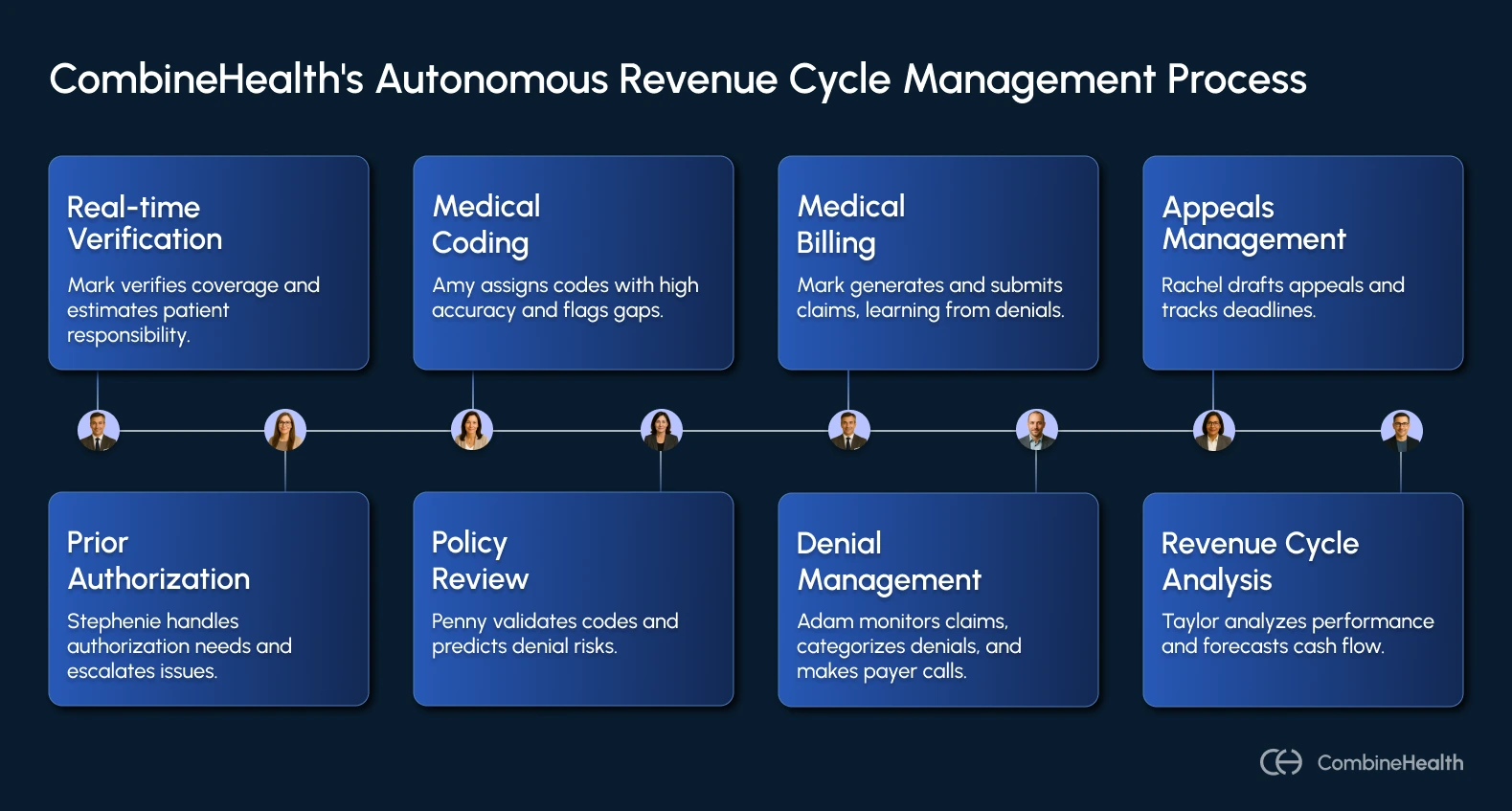
AI sits across intake, documentation, coding, and claims workflows to automate repetitive work, predict risk, and prevent errors before they become denials. Instead of reacting downstream, AI enables proactive control upstream.
Here are some key AI use cases across the healthcare revenue cycle:
- Autonomous medical coding: AI models can read clinical documentation, extract relevant clinical concepts, and suggest accurate ICD-10, CPT, and modifier combinations.
- Predictive denial prevention: Rather than waiting for payer rejections, AI can analyze claims before submission and score them for denial risk.
- Eligibility and benefits automation: AI automates real-time eligibility and benefits checks during scheduling and intake, where many denials originate.
- Clinical documentation integrity checks: AI can continuously review clinical notes against payer-specific medical necessity rules, flagging missing specificity and documentation gaps.
- Automated claims routing and payment posting: Beyond intelligence, AI and RPA can also handle execution. This includes submitting claims across clearinghouses and payer portals, reading ERAs and EOBs, and posting payments automatically, and reconciling expected vs. actual reimbursement.
How Does Patient Intake and RCM Go Hand In Hand?
Patient intake isn’t a parallel administrative process—it’s the first step of the revenue cycle. Everything that happens downstream in RCM is built on the data captured at intake. In fact, CMS shows that a large share of improper payments in Medicare, Medicaid, and CHIP are driven by “insufficient documentation” and “eligibility/coverage issues,” not just bad codes.
Here’s why intake and RCM are inseparable:
- Intake data is the raw material for every claim: Demographics, insurance details, eligibility status, and authorizations all feed directly into coding, billing, and payer validation.
- Errors at intake don’t stay isolated: A wrong policy number or missing authorization doesn’t just affect registration—it cascades through documentation, coding, claim creation, and collections.
- Front-end accuracy drives back-end performance: Digital intake that verifies eligibility and enforces complete data capture produces cleaner claims and higher first-pass payment rates.
Using AI across the lifecycle allows organizations to:
- Reduce front-end denials
- Improve mid-cycle accuracy
- Generate error-free claims before submission
Resilience Comes from Strengthening the System End-to-End
Financial resilience in healthcare doesn’t come from fixing denials faster or chasing payments harder. It comes from strengthening the systems that determine whether revenue survives in the first place.
That starts with patient intake, and it continues with revenue cycle management.
When intake is weak, the revenue cycle spends its time cleaning up preventable problems. When RCM is weak, even good intake data fails to convert into cash. But when both are strong, clinics see cleaner claims, faster payments, fewer denials, and more predictable cash flow.
If you want to see how CombineHealth AI solutions can make your RCM workflow strong, book a demo with us!
Related Posts
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
Subscribe to newsletter - The RCM Pulse
Trusted by 200+ experts. Subscribe for curated AI and RCM insights delivered to your inbox
Let’s work together and help you get paid
Book a call with our experts and we'll show you exactly how our AI works and what ROI you can expect in your revenue cycle.
Email: info@combinehealth.ai





.webp)











